Chronic conditions such as Inflammatory Bowel Disease (IBD) affect a significant portion of our population, impacting individuals’ health and quality of life. Understanding IBD – its causes, symptoms, complications, and the treatments available, including Surgery For Ulcerative Colitis and Chrohns Disease, can be incredibly beneficial for those affected by the disease and their families.
For those affected this article aims to shed light on the array of surgical procedures for IBD, explaining when and why they may become necessary. This includes an extensive discussion on colectomy, proctocolectomy, and ileoanal anastomosis, among others.
Recognizing the advantages and potential pitfalls of surgery for Ulcerative colitis and Crohn’s Disease can aid in informed decision-making about the best course of treatment. Besides, a thorough understanding of the surgical process, appropriate lifestyle management, and requisite follow-up care can abet individuals in navigating life pre and post-surgery, thereby pushing the boundaries of their potential altogether.
Surgery For Ulcerative Colitus and Chrohns Disease
Understanding IBD In Its Two Main Forms
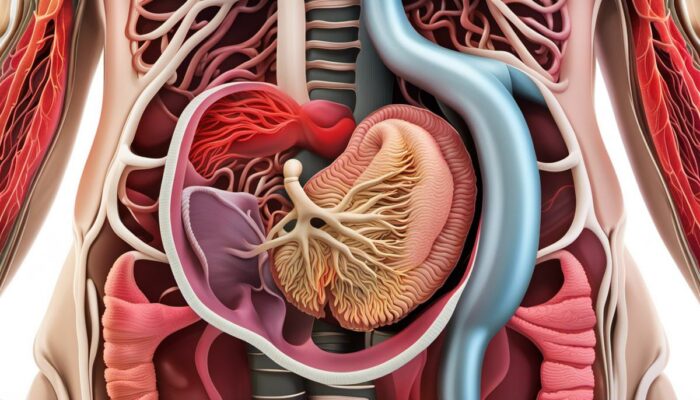
Inflammatory bowel disease (IBD) comprises two major types: Crohn’s disease and ulcerative colitis. Both disorders result from abnormal responses of the body’s immune system, attacking the gastrointestinal (GI) tract’s lining and causing chronic inflammation.
The exact causes of IBD, regrettably, remain unknown. However, scientists theorize that it may be due to a combination of genetic, immune system, and environmental factors.
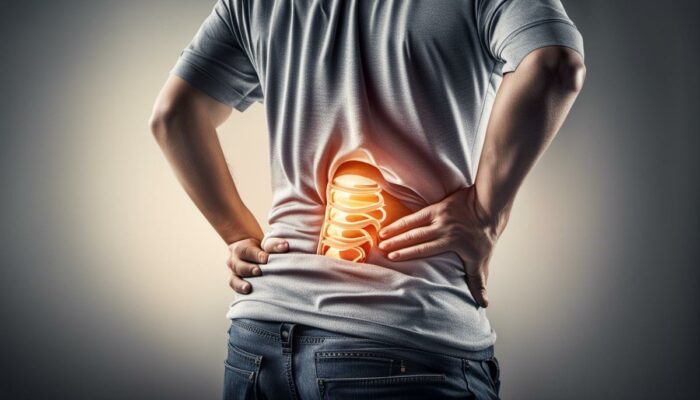
Symptoms of IBD can vary widely, depending on which part of the GI tract is affected and the severity of the inflammation. Common signs include;
- Diarrhoea,
- Abdominal Pain and cramping,
- Blood in your Stool,
- Reduced Appetite and
- Unexplained weight loss.
- In severe cases, individuals may also experience fever, fatigue, and anemia.
IBD can fluctuate between periods of flare-ups, during which symptoms are active, and remission, in which symptoms disappear. It’s also worth noting that IBD isn’t limited to the GI tract and can sometimes involve complications affecting the joints, eyes, skin, and liver.
Complications of IBD
Long-term inflammation and ulcers in the rectum and colon are common for patients with IBD, especially in those suffering from ulcerative colitis. These sores might bleed, leading to blood in the stool, and can even form fistulas – abnormal connections or passageways between different body parts.
IBD increases the risk of colon cancer, particularly in individuals with extensive inflammation. The risk is further amplified in those who have had IBD for eight years or more.
Other complications can include bowel obstruction, malnutrition, anaemia, osteoporosis, and other health concerns related to the effects of chronic inflammation.
Understanding the Role of Surgery in IBD Management
Surgery is considered an alternative treatment for individuals living with IBD when medicinal therapies no longer provide relief, complications emerge or the risk of cancer intensifies. Surgical procedures are typically more prevalent in individuals diagnosed with ulcerative colitis, compared to those with Crohn’s disease, due to the localized characteristics of ulcerative colitis.
The specific surgery conducted heavily relies on the category of IBD, along with the severity of the condition. For instance, in ulcerative colitis, a medical procedure like proctocolectomy – complete removal of the colon and rectum – may be undertaken, frequently followed by the construction of an ‘ileal pouch’ to act as a replacement for the rectum.
For individuals diagnosed with Crohn’s disease, the surgical procedure may include the removal of only the diseased parts of the GI tract, ensuring the healthy parts remain unaffected.
However, surgery does not guarantee to cure Crohn’s disease – inflammation often reappears in different parts of the GI tract over time.
The decision to undergo surgery for IBD treatment demands careful thought about the advantages and potential risks. This process should include close consultation with your medical team. Every case of IBD is unique; therefore, the optimal treatment for one person may not necessarily be the most effective for another. For this reason, a thorough understanding of IBD and thorough discussions of all treatment options with your doctor are crucial.
An Overview of Surgical Interventions for IBD
Inflammatory bowel disease (IBD), a term that encompasses Crohn’s disease and ulcerative colitis, manifests through uncontrolled inflammation within the digestive tract. For severe forms of IBD, surgical procedures may be necessary either to manage persistent symptoms or address serious complications such as blockage, bleeding, and perforation.
Some of the frequently performed surgical interventions for IBD include colectomy, proctocolectomy, and ileoanal anastomosis. Each of these surgical procedures I shall further explain below.
Colectomy
A colectomy involves the removal of all or part of the colon and can be indicated for individuals with colonic IBD refractory to medical treatment, or for those suffering from serious complications like severe bleeding. There are various types of colectomies: a total colectomy (removal of the entire colon), a partial colectomy (removal of part of the colon), and a proctocolectomy (removal of both the colon and rectum).
For example, a subtotal colectomy, which removes most but not all of the colon, is generally performed on patients with disease limited to the colon itself. There may still be potential for disease recurrence in the remnant colon, and it might necessitate further future surgeries.
Proctocolectomy
A proctocolectomy, which involves removal of both the colon and rectum, is typically indicated for patients with severe IBD affecting the entire colon and rectum, or when there is a risk of cancer. The procedure is often completed with either ileostomy (an external bag to collect waste) or ileoanal anastomosis.
Ileoanal Anastomosis
The ileoanal anastomosis also referred to as ileal pouch-anal anastomosis (IPAA), is often performed following a proctocolectomy. This procedure involves the creation of a pouch from the last part of the small intestine, which is then connected to the anus to restore intestinal continuity and allow the patient to pass waste naturally. The procedure is often done in two stages, allowing the newly formed pouch to heal before it becomes functional.
To conclude
The nature of the surgical procedure recommended is influenced by factors such as the severity of IBD, the individual’s overall physical wellness, and the specific locations of the digestive tract affected. Discussing the advantages and disadvantages of each surgical option with healthcare providers is vital for patients.
Obtaining a second opinion, if necessary, is also a sound course of action. Further, it must be acknowledged that while surgery can often provide substantial relief from symptoms, it is by no means a definitive cure for IBD. Chronic healthcare management and lifestyle modification remain integral aspects of managing IBD.

Benefits and Risks of IBD Surgery
Understanding IBD Surgery
Inflammatory Bowel Disease (IBD), a collective term that includes conditions such as Crohn’s Disease and Ulcerative Colitis, often results in appreciable discomfort and can interfere significantly with everyday life. When treatments centred around medication fail to provide effective relief, surgical options may be explored. This course of action can have a considerable positive impact by easing symptoms and enhancing the patient’s quality of life. However, as with most major medical procedures, it is also associated with potential risks and complications.
Benefits of IBD Surgery
One of the key benefits of opting for surgery is symptom relief, which can lead to a substantial boost in the patient’s Quality of Life (QoL). IBD conditions can cause severe abdominal pain, fatigue, and diarrhoea – making everyday activities a struggle. Post-surgery, many patients experience a significant reduction, if not complete elimination of these symptoms.
One form of IBD surgery, colectomy – the removal of some or all of the colon – can be a definitive cure for Ulcerative Colitis, thereby eliminating the need for ongoing drug therapy. In other cases, surgery may not provide a complete cure but can enable the patient to reduce or suspend their medication, which can enhance their quality of life.
Moreover, opting for surgery could prevent the progression of the disease and associated complications, thereby avoiding emergencies that necessitate immediate surgery.
Risks and Complications of IBD Surgery
Despite these benefits, it’s important to consider the potential risks and complications of IBD surgery. All surgical procedures carry inherent risks such as infections, blood clots, or adverse reactions to anaesthesia.
Specific to IBD surgery, potential complications could include pouchitis (inflammation of the ileal pouch, a common side-effect of surgery for Ulcerative Colitis), malabsorption of nutrients or dehydration as a result of intestine removal, and sexual dysfunction resulting from nerve damage during surgery.
Moreover, in the case of Crohn’s Disease, IBD surgery treats the symptoms rather than curing the disease itself. This means that while the surgery might bring temporary relief, the disease could recur in another part of the digestive tract.
Surgical Success Rates and Patient Testimonials
Surgical success rates for IBD vary depending on patient factors and the specifics of each case. For example, Ileal Pouch-Anal Anastomosis (IPAA), a common surgery for Ulcerative Colitis, has a success rate of 85-90% at controlling the disease without the need for ongoing medication.
Patient testimonials often highlight the transformative effect surgery can have, citing significant improvements in daily living, renewed energy levels, and the liberation from debilitating symptoms. However, patients also stress the importance of considering the possible complications and ensuring the decision to proceed with surgery is well-considered, made in consultation with a qualified healthcare professional.
The Choice Is Individual
In conclusion, opting for IBD surgery is a deeply personal decision that should be based on the specific circumstances of the individual. It involves balancing the potential benefits – the alleviation of symptoms, enhanced quality of life, and possible disease resolution – against the risks and potential complications.
Consulting with healthcare professionals and hearing from other patients who have undergone the procedure can be invaluable in helping to make an informed decision.
The Process of Surgery: Pre, During, and Post-Operative Care
Living with IBD Post-Surgery: Lifestyle Management and Follow-Up Care
Post-IBD Surgery Lifestyle Management
The quality of life after surgery for inflammatory bowel disease (IBD) largely depends on how individuals manage their lifestyle. This can typically include a combination of dietary changes, physical activity, medication, and regular follow-ups with healthcare professionals.
Post-surgery dietary alterations are often recommended to aid the healing process and maintain overall health. Patients may be advised to have small, frequent meals rich in protein and low in fibre to avoid irritation of the digestive tract. However, dietary requirements could vary from person to person, hence consultation with a dietitian can provide personalised guidance.
Physical activity post-surgery can assist in speeding up recovery, boosting the immune system, and promoting overall well-being. Yet, it is crucial for patients to discuss their exercise regimen with a healthcare provider, as too much physical strain too soon after surgery might lead to complications.
Long-term medication management is another key component of post-surgery care. Many IBD patients will need to continue taking medication to control inflammation and manage symptoms. Compliance with the prescribed medication regimen is vital for controlling IBD in the long run. Some individuals might also require vitamin or mineral supplements to ensure nutritional adequacy.
Follow-up Care
Regular follow-ups play a pivotal role in monitoring the effectiveness of treatment, catching early signs of relapse, and adjusting medications accordingly. They also provide an opportunity for patients to discuss any concerns or issues related to their condition or treatment.
Emotional Impact of Surgery and Psychological Support
It’s important to highlight that the journey post-IBD surgery is not just physical, but also emotional. Many individuals may experience feelings of relief once the surgery is over, but they might also struggle with fears about recurrence, body image issues, or anxiety about managing their condition.
Psychological support forms a crucial part of the post-surgery care framework. Counselling, or therapy can help individuals cope with the emotional impact of IBD and surgery. Connecting with support groups, both offline and online, can offer a space to share experiences and learn from others who have gone through similar journeys.
In conclusion, life after IBD surgery can indeed pose challenges, but with careful lifestyle management, regular follow-ups, and the right emotional support, patients can lead healthy, fulfilling lives. The holistic management of IBD post-surgery underscores the fundamental concept of blended care, where attention is given to the physical and emotional well-being of individuals.

No journey with a chronic condition is easy, especially when surgical intervention becomes necessary. Dealing with IBD can feel daunting and the thought of surgery might be daunting, but understanding the entire process can indeed empower patients to take control of their health.
From explaining the necessity and types of surgical procedures for IBD, their associated benefits and risks, and what to expect during preoperative, operative, and postoperative stages, this discourse has aimed to equip individuals with comprehensive knowledge.
Above all, adopting the necessary lifestyle modifications post-surgery and getting the needed psychological support inevitably makes a drastic difference in adjusting to a new normal.
Although the path may seem challenging, with the right information, guidance, and support, a fulfilling life is certainly achievable for individuals dealing with IBD, even post-surgery.
Anxiety and Depression best ways to lower blood sugar BiOptimizers blood pressure supplements blood sugar support supplements Digestive Enzymes Supplement digital products Dr Sam Robbins Erectile dysfunction Exercise Gut Health Healthy Living heart health HFL how to lower blood sugar levels How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance list Magnesium deficiency Matt Gallant mental health multivitamins Nootropics nutrient supplements Probiotics Probiotic Supplements proteolytic enzymes reverse type 2 diabetes stress and anxiety stress relief vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss supplements that work weight loss tea