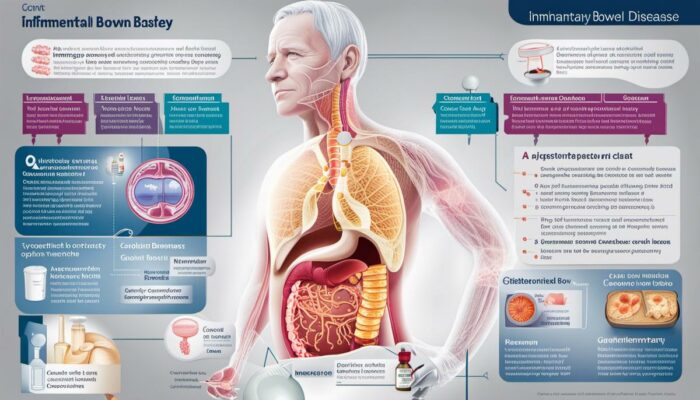
There is a rising need to shed light on a growing health concern, Inflammatory Bowel Disease (IBD) which affects several individuals worldwide. This condition epitomizes the struggle between man and his own body, with IBD being embodied as an internal physical conflict. With types such as Crohn’s disease and ulcerative colitis, IBD is not just a singular problem, but a spectrum of disorders that impacts every patient differently.
Comprehending the multifaceted nature of IBD, appreciating its symptoms, and understanding how it’s diagnosed are all vital steps in learning to live with, manage, or even aid those who endure this health challenge. This article will provide crucial insights while exploring the array of differing treatments currently available.
Understanding Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) is not a single disease but a term that encompasses several chronic diseases that cause inflammation of the gastrointestinal tract (GIT). These GIT disorders are defined by the area of the digestive tract they affect and are chronic conditions with periodic flare-ups that can impact an individual’s quality of life.
Symptoms of IBD
The symptoms of both Crohn’s Disease and Ulcerative Colitis can be similar and may include abdominal pain, cramping, diarrhea, nausea, fatigue, weight loss, and reduced appetite. These symptoms can range from mild to severe, and the duration of these symptoms can also vary greatly. People with IBD may also experience periods of remission, where the symptoms lessen or disappear completely for a while.
Treatment for IBD
There is a wide range of treatment options available for IBD, with the choice of treatment often depending on the type and severity of the condition, the affected area of the GIT, and the individual’s overall health and lifestyle.
Medication
Medications for IBD primarily aim to reduce inflammation and thereby relieve the symptoms. These may include anti-inflammatory drugs, immunosuppressants, corticosteroids, and biological therapies, each with its own potential benefits and side effects.
Surgery
In some cases, when medication and other treatments are not effective, or if complications arise, surgery may be recommended. For Crohn’s disease, surgery can provide temporary relief but is generally not considered a cure. However, for Ulcerative Colitis, surgery to remove the colon can effectively treat the condition, but comes with its own set of potential issues including the need for a stoma or an internal pouch to collect waste.
Diet and Lifestyle Adjustments
Many individuals with IBD may find that specific foods or beverages trigger or worsen their symptoms. Therefore, dietary changes may play a significant role in managing IBD symptoms. Reducing the intake of certain foods like dairy products, high-fiber foods or fatty foods might be advised. Regular exercise and sufficient sleep can also positively impact the overall health and well-being of individuals with IBD.
Psychological Support
Given the chronic nature of the disease and the impact it can have on the individual’s quality of life, psychological support is often a crucial part of the treatment plan. This can include counseling, support groups, and stress management techniques.
It’s crucial to understand that each individual’s journey with Inflammatory Bowel Disease (IBD) is distinct, and teaming up with healthcare professionals to identify the most efficient and effective treatment plan is the key to coping with this chronic illness.
Symptoms and Diagnosis: Identifying IBD
IBD typically affects your daily routine by causing a variety of physical discomforts. Common symptoms include persistent diarrhoea, blood in the stool, fever, loss of appetite, and a noticeable reduction in energy levels. Many people may also experience dramatic weight loss over a short period as the digestive system struggles to absorb nutrients effectively.
Moreover, IBD often triggers complications beyond the confines of the digestive system. Frequent issues include arthritis, eye complaints, skin rashes, and mouth sores. These are usually observed in line with IBD flare-ups. Additionally, some patients have noted instances of compromised liver function, kidney stones, osteoporosis and, though quite rare, cancer.
Patients’ Experiences with IBD
The personal experiences of patients living with IBD reflect the extensive impact it has on their lives beyond the mere physical manifestations. Chronic fatigue, joint pain, and dependency on medications are some of the common threads shared. Reports of mental health struggles co-existing with the disease, such as anxiety and depression, are also widespread due to the unpredictable nature and debilitating consequences of its symptoms. Furthermore, many patients experience social ostracisation and find it challenging to maintain an active lifestyle, affecting their relationships and work life.
Diagnosing IBD
Diagnosing IBD involves an array of tests and procedures to exclude the possibility of other conditions with similar symptoms. Initial evaluations may include blood and stool tests to check for infections, inflammations, and other abnormalities in the body, such as anemia.
Medical professionals employ imaging techniques such as colonoscopy, MRI, and CT scans for a detailed view of the gut and surrounding tissues. A colonoscopy can provide the most accurate diagnosis as the camera enters the rectum to capture images and allows the doctor to take tissue samples for biopsy.
Doctors may also resort to special video capsule swallow tests for a close-up view of the small intestine, which traditional colonoscopies might not reach.
IBD Treatment Options
Treatment for IBD focuses on reducing inflammation, managing symptoms, and reducing the frequency of flare-ups, thereby aiming to improve the patient’s quality of life. Medication is often used as a frontline treatment option. Aminosalicylates, corticosteroids, and immunosuppressants serve to diminish inflammation, while antibiotics can treat or prevent secondary infections.
In cases where the disease shows intolerance or resistance to medication, surgery might become necessary. Though viewed as the last resort, surgical procedures — particularly colectomy, the removal of the colon — can sometimes resolve symptoms entirely.
The introduction of biological therapies has revolutionized IBD treatment in recent times. Biologics, drugs derived from living organisms, target specific proteins causing inflammation, offering promising results.
IBD management doesn’t stop at medication. Lifestyle changes, including dietary modifications, stress reduction, and routine exercise, play a crucial role in managing the symptoms of this chronic illness. Some patients exhibit favorable responses to exclusion diets, probiotics, and even hypnotherapy.
Advancements in IBD Treatment
Drug developers consistently strive to discover advanced treatments for Inflammatory Bowel Disease (IBD), prioritizing anti-inflammatory and immunosuppressive drugs. As technology advances, the possibility of personalized treatments based on genetic and microbial factors emerges, indicating a potential future where individualized treatment plans can be created to suit each patient’s unique needs.

Current IBD Treatments
Managing Ulcers in IBD
In the context of IBD, ulcers are generally managed with medication aimed at controlling inflammation and promoting tissue repair. Frequently prescribed medications include aminosalicylates such as mesalamine or sulfasalazine, which are renowned for their anti-inflammatory capabilities. Corticosteroids also play a crucial role in the management of inflammation, although they are typically reserved for short-term use or acute cases due to potential side effects, including an increased risk of infection and bone density reduction. Despite the significant benefits of these drugs, potential side effects ranging from mild symptoms like nausea and headache to severe complications such as heightened infection risk should be considered.
Steroid-based Treatments in IBD
Steroid-based treatments for IBD, like prednisolone, are commonly used for moderate to severe disease flare-ups. They work by suppressing the immune system, reducing inflammation in the digestive tract. Although they can be highly effective in managing symptoms, long-term use of steroids can lead to serious side effects. These may include osteoporosis, high blood pressure, diabetes, and an increased susceptibility to infections. As a result, steroids are usually reserved for short-term use or as a last resort treatment option when other methods have proven ineffective.
Immunosuppressants in IBD Management
Immune system suppressors, or immunosuppressants, are another treatment option for IBD. They work by reducing the immune system’s inflammatory response, which can help control symptoms and reduce the risk of complications. Commonly used immunosuppressants for IBD include azathioprine and mercaptopurine. While they are effective in controlling symptoms, they can also increase the risk of infections and cause side effects like nausea and fatigue.
Surgical Procedures for IBD
Surgery is an option for more severe cases of IBD and may be necessary if medication-based treatments are ineffective. The procedures will vary depending on whether the patient has Ulcerative Colitis or Crohn’s disease. In Ulcerative Colitis, a colectomy, removal of the entire colon, may be performed. In Crohn’s disease, sections of the damaged intestine may be removed in a procedure known as a resection. In both instances, there can be significant improvements in the quality of life, though they do not cure the condition and can have complications like infections or a change in bowel habits.
Biologics for IBD Treatment
Biologic treatments are one of the newer options available for IBD. They work by blocking specific proteins in the body that cause inflammation, thereby reducing symptoms. Anti-TNF agents like infliximab are most commonly prescribed, and can be very effective. Though biologics have revolutionized the treatment of IBD, they do have potential side effects including reactivation of dormant infections like tuberculosis and an increased risk of certain cancers. Moreover, not every patient responds well to biologics, and their high cost can be prohibitive.
The complexity of IBD treatment options ranges from the use of ulcers to advanced biologic treatments, all of which carry their own sets of advantages and disadvantages. The best fitting treatment for an individual hinges upon a few key factors. These include the severity of their symptoms, their specific type and the extent of Inflammatory Bowel Disease (IBD), as well as their unique response to an array of medications.

Role of Diet & Lifestyle in IBD Management
The Critical Contribution of Diet in Managing IBD
The management of Inflammatory Bowel Disease (IBD) is significantly influenced by one’s diet, though it bears no direct link to causing or curing the condition. The incorporation of a balanced and nutritious diet can, however, assist in alleviating symptoms, supplying essential nutrients, and bolster one’s general wellbeing. The significance of maintaining a well-rounded diet cannot be overstated. It’s strongly advisable to incorporate a mixed diet that includes lean proteins, whole grains, fruits, vegetables and low-fat dairy products, aiming to ensure adequate nutrient intake and to encourage better health in general.
Of note though, is that each individual living with IBD is likely to have a distinctive set of foods that could aggravate their symptoms—these ‘trigger foods’. These types of food can drastically vary between individuals and are best discovered through careful and detailed observation and record-keeping. The most commonly identified triggers often encompass spicy or fatty foods, dairy products, foods high in fibre or even drinks that are caffeinated or alcoholic.
Importance of Regular Exercise in IBD Management
While physical activity might seem challenging during an IBD flare-up, maintaining a consistent exercise routine can prove beneficial in managing the symptoms. Regular exercise improves your overall health, enhances the immune system and reduces inflammation. Besides, it can also alleviate stress and bolster your mood, playing an essential role in your psychological wellbeing.
However, the choice of exercise is important. Low impact exercises such as walking, swimming or gentle yoga can provide the health benefits required without aggravating the symptoms of IBD. It is necessary to recognise your body’s limit and adapt your workout routine as needed, keeping in mind the varying phases of the disease.
Stress Management and the Connection with IBD
Stress doesn’t directly cause IBD, but there is a clear stress-IBD connection, with stress being able to worsen IBD symptoms. Though everyone has stress, people with IBD might find their symptoms flaring up during high-stress periods. This necessitates the significance of stress management for individuals with IBD.
Effective stress management techniques can include mindfulness, meditation, and breathing techniques, all of which can help to reduce stress levels, and thereby potentially improve your IBD symptoms. Engaging in enjoyable activities or hobbies, ample sleep, staying connected with loved ones, or seeking help through therapy or support groups can also help manage stress.
To effectively manage Inflammatory Bowel Disease (IBD), it is crucial to focus on diet and lifestyle modifications. These may encompass maintaining a balanced diet, engaging in regular low-impact exercises, and effectively managing stress. While these strategies may not cure IBD, they can significantly help in reducing symptoms and improving the overall quality of life of those affected. However, personalised advice from healthcare professionals must be sought before initiating any new diet or exercise programme.
Future Developments in IBD Treatment
The Advent of Personalised Medicine
In the continuously evolving landscape of IBD treatment, there’s a bright ray of hope that emerges from the field of personalised medicine. This pioneering approach leverages the unique genetic information of an individual to design treatment plans that are tailored specifically to the patient’s unique needs. Genetic profiling provides insights into a person’s susceptibility to IBD, their potential response to specific treatments, and the likelihood of experiencing various side effects, paving the way for more effective and individualised care.
Exploring Gut Microbiota
Significant research is underway focusing on the gut microbiota, aiming to understand the interplay between gut flora and IBD. The gut microbiota is the huge collection of microorganisms that inhabit the human gastrointestinal tract. These microbes are critical for human health, affecting everything from nutrient absorption to immunity. In individuals suffering from IBD, the composition of the gut microbiota is often out of balance. Restoring this balance, potentially through next-generation probiotics, prebiotics or transplant of healthy fecal matter, represents an exciting treatment avenue.
Novel Pharmacological Targets
Advances in the understanding of IBD pathogenesis have unveiled several novel targets for therapeutic intervention. These discoveries are fuelling the development of a new range of drugs to combat IBD. Interleukin-based therapies, such as IL-12 and IL-23 inhibitors, are one such group of drugs that are showing positive preliminary results in IBD treatment. These drugs target specific immune cells, reducing inflammation in the gut tissues.
Stem Cell Therapy
Stem cell therapies are an area of research that is attracting growing interest for the treatment of IBD. Mesenchymal stem cells, in particular, are the subject of extensive pre-clinical and clinical investigation due to their anti-inflammatory properties. They also have the potential to repair damaged tissue, offering the tantalising possibility of potentially being able to heal the chronic tissue damage caused by IBD.
The Promise of Nucleotide Analogs
Nucleotide analogs, such as thymoquinone, have recently surfaced as an effective treatment option for IBD. By mimicking certain biochemical structures, these analogs have the ability to influence the body’s biological processes in beneficial ways, such as reducing inflammation or boosting healing responses.
In Conclusion
Across the globe, research into innovative treatments for IBD is advancing at a rapid pace. From personalized medicine and novel drug targets to explorations of gut microbiota and stem cell therapies, scientists and clinicians are making significant strides toward finding a cure for IBD.
As these pioneering treatments continue to evolve, there is substantial hope for patients suffering from these debilitating conditions. As members of the public, witnessing these developments underscores the power and potential of modern medicine.
Beyond providing hope for the future, it serves as a testament to human ingenuity and the relentless quest for knowledge and understanding.

Unswerving strides are being made in the field of IBD research, with medical scientists and researchers tirelessly working towards unveiling safer and more efficient treatment options. Their efforts range from refining existing solutions to delving into the exciting realm of personalized medicine.
Highlighting the promise shown by novel therapies, we await a future where managing IBD may not be as grueling a task as it can often be today. Moreover, each individual’s role in controlling IBD through diet and lifestyle changes should not be underestimated, for it is often these modifications that form the bedrock of long-term management.
As we get a glimpse of what the future holds, it is critical to remember that while IBD is an incredibly complex disorder, hope is on the horizon. {Read More about IBS and IBD HERE<<}
