Inflammatory Bowel Disease (IBD) is a term that encompasses a number of conditions characterized by inflammation within the digestive tract, with the most common forms being Ulcerative Colitis and Crohn’s disease. For individuals affected by these conditions, everyday life can often be a struggle, where both acute flare-ups and chronic symptoms significantly impact their quality of life.
A central part of this discussion, and an arena of growing research interest is the role of antibiotics in the management of these conditions. Besides their primary role in combating bacterial infections, antibiotics have been found to play several pivotal roles in the treatment of IBD, from mitigating intestinal inflammation to restoring gut health.
This examination serves as a comprehensive exploration of their role, including the associated benefits and potential risks.
Understanding the Role of Antibiotics in IBD Management
Overview of IBD
Inflammatory Bowel Disease (IBD) constitutes a group of chronic intestinal disorders typified by persistent and recurring inflammation of the digestive tract. The two most common forms of IBD are Crohn’s Disease and Ulcerative Colitis.
Herein, Crohn’s Disease incites inflammation anywhere in the digestive tract, from the mouth to the anus, and can penetrate into the deep layers of tissues. Conversely, Ulcerative Colitis primarily affects the lining of the large intestine (colon) and rectum, with inflammation occurring in adjoining areas.
Symptoms of IBD oscillate between severe and mild, and often manifest in episodes or ‘flare-ups’. Common symptoms include chronic diarrhea, abdominal pain, rectal bleeding, weight loss, and extreme fatigue.
However, IBD can also trigger symptoms unrelated to the digestive system, encompassing skin rashes, joint pain, and eye irritations. The exact cause of IBD is unknown, though most theories propose it precipitates from an unwarranted immune response to factors like genetics, diet, stress, or infections.
Role of Antibiotics in Managing IBD
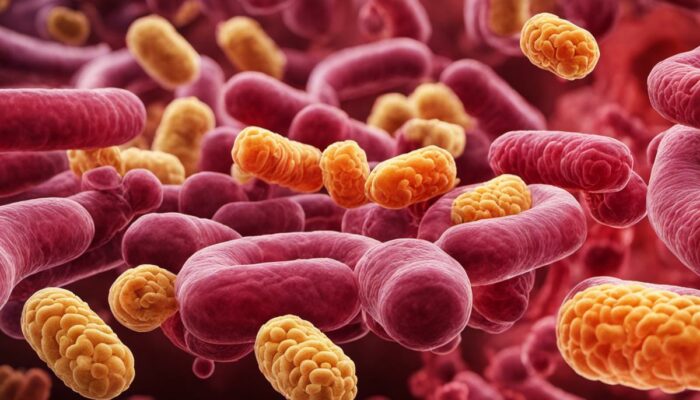
In the management of Inflammatory Bowel Disease (IBD), antibiotics figure significantly. Our gut is home to an array of microorganisms, collectively known as gut microbiota, crucial for maintaining digestive health. Any disruption to this community, referred to as dysbiosis, is a characteristic of IBD, culminating in an inflammatory atmosphere within the gut.
This is where antibiotics come into play. These medications have the power to redress the balance of gut microbiota by suppressing harmful bacteria, thereby lessening inflammation and alleviating IBD symptoms.
Antibiotics like Metronidazole and Ciprofloxacin have shown substantial efficacy in treating IBD, notably in individuals with Crohn’s disease involving the perianal area or those with highly active ulcerative colitis. By reducing intestinal inflammation, these antibiotics can contribute to enhancing the patient’s overall well-being.
However, antibiotics must be used judiciously. Extended use may result in antibiotic resistance along with potential side effects like nausea, photosensitivity, and in certain instances, severe diarrhea.
Consequently, antibiotic therapy is often implemented as a temporary measure, in conjunction with other treatments such as anti-inflammatory medications.
Emerging research is probing the impact of combining antibiotics with probiotics, which could lead to highly personalized treatment plans and more effective management of IBD in the future. However, it’s important to recognize that the impact of antibiotics in IBD treatment may vary from person to person, thereby necessitating customized treatments based on each individual’s specific needs.
Antibiotics and Their Functionality
Decoding Antibiotics
Antibiotics are antimicrobial drugs meant to treat and ward off bacterial infections. They work by either eradicating bacteria or inhibiting their propagation. However, antibiotics are powerless against viral infections like the flu or the common cold.
The broad categories of antibiotics comprise penicillins, cephalosporins, macrolides, fluoroquinolones, sulphonamides, tetracyclines, and aminoglycosides, among others.
Each category is effective against distinct types of bacteria, and their mechanisms of action differ as well. Some antibiotics, categorized as broad-spectrum antibiotics, are capable of targeting a wide range of bacteria, whilst others, classified as narrow-spectrum antibiotics, only act against specific types of bacteria.
Antibiotics and Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) encompasses conditions characterized by chronic or recurring immune response and inflammation of the gastrointestinal tract. The two most common diseases in IBD are Crohn’s Disease and Ulcerative Colitis.
While the cause of IBD is yet to be definitively determined, it is thought that a malfunctioning immune system, genetics, lifestyle factors, and environmental triggers all play a role. One such environmental trigger might be the gut microbiota – the community of microbes that live in our digestive tract.
The use of antibiotics in IBD is predicated on the understanding that the inflammation seen in IBD might be driven or aggravated by an imbalance in the gut microbiota, known as dysbiosis, or by specific pathogenic bacteria. In this scenario, antibiotics can help by reducing the number of potentially harmful bacteria and rebalancing the gut microbiota.
Efficacy of Antibiotics in IBD Treatment
Several antibiotics, including Metronidazole, Ciprofloxacin, and Rifaximin, have been shown to be effective in managing certain aspects of IBD. For instance, metronidazole and ciprofloxacin are often used in treating perianal disease in Crohn’s, while Rifaximin has shown some promise in inducing remission in Ulcerative Colitis.
However, the role of antibiotics in IBD isn’t entirely clear-cut. Some research suggests that overuse of antibiotics, particularly in childhood, may increase the risk of developing IBD, possibly by perturbing the gut microbiota. Moreover, long-term antibiotic use can lead to antibiotic resistance, a serious global health concern.
Answer
To summarise, antibiotics play a key role in the management of numerous elements of IBD. However, their administration should be judicious and under the supervision of a competent healthcare professional. Further studies on the specific involvement of the gut microbiota in IBD and the possible medication effects of antibiotics or other therapies targeting microbiota are needed.
In addition to this, a larger focus on maintaining a balanced and diverse gut microbiota possibly through changes in diet and lifestyle or the utilization of probiotics, could play a fundamental role in the prevention and treatment of IBD.

Antibiotics in IBD Treatment
Impact of Antibiotics on IBD Treatment
Antibiotics are a recognized component in the management of inflammatory bowel disease (IBD), a collective term comprising conditions like Crohn’s disease and ulcerative colitis. These enduring disorders affect the gastrointestinal tract, triggering symptoms such as diarrhea, weight loss, and stomach pain. In dealing with these diseases, antibiotics fulfill numerous fundamental roles.
Reducing Intestinal Inflammation
One primary purpose of antibiotic use in IBD treatment is to decrease the inflammation in the intestine. Inflammation is a cornerstone characteristic of IBD, and its reduction is central to relieving symptoms. Antibiotics work by reducing the augmented levels of harmful bacteria in the gut that can provoke an inflammatory reaction. Therefore, they contribute to alleviating the intensity of IBD flare-ups, enhancing the patient’s overall comfort.
Restoring Gut Flora Balance
In harmony with reducing inflammation, antibiotics also play a crucial role in restoring normal balance to the gut microbiota. The delicate balance in gut flora is necessary for healthy digestion, but IBD often disrupts this equilibrium, leading to excessive harmful bacteria.
Antibiotics target these problematic bacteria and control them, thereby enabling healthier, beneficial bacteria to propagate and recreate a balanced gut environment. This, then, supports the natural defense mechanisms of the gut against IBD.
Addressing Related Complications or Surgical Interventions for IBD
Beyond managing the primary symptoms and effects of IBD, antibiotics are also critical in mitigating complications or surgical interventions. IBD patients frequently experience complications like fistulas and abscesses, and antibiotics can help treat these conditions by killing bacteria that can contribute to these complications.
Furthermore, before surgical interventions are used to manage IBD, antibiotics are often administered to reduce the risk of infections post-surgery.
Adjunctive Use of Antibiotics with Other IBD Therapies
Although antibiotics can significantly contribute towards addressing IBD, they are often used in combination with other IBD therapies for a holistic approach. They can improve the effectiveness of other treatments by maintaining a balanced gut flora and reducing inflammation, creating an environment conducive to healing.
Notably, antibiotics can help increase the effectiveness of immunomodulators and biological therapies, which are often vital components of IBD treatment.
In conclusion
Antibiotics occupy a significant position in handling IBD. They play multiple roles, from reducing inflammation and maintaining a balanced intestinal flora to assisting in the management of complications or surgical procedures. These drugs are therefore a key component in a comprehensive IBD treatment plan, complementing other therapies by providing patients with a multifaceted and effective treatment strategy, thus greatly contributing to advancements in managing IBD.
Review of Relevant Research Findings
Inflammatory Bowel Diseases (IBDs), primarily Crohn’s disease and ulcerative colitis, are long-term conditions causing inflammation in the digestive tract, and their causes are multiple and complex. Antibiotics emerge as critical in addressing these conditions, offering benefits such as modulating the deleterious bacteria population within the gut, lowering inflammation, and effectively treating fistulas and abscesses that characterize Crohn’s disease.
Research findings suggest the effectiveness of antibiotics in managing IBD. Within the spectrum of inflammation, certain bacteria overgrow and cause dysbiosis that can instigate or perpetuate the inflammatory state. Antibiotics, by controlling the overgrowth of detrimental bacteria, can help restore balance in the gut microbiota, possibly alleviating symptoms and controlling disease progression.
The antibiotics predominantly used for IBD management include metronidazole, ciprofloxacin, and rifaximin. Metronidazole and ciprofloxacin have been shown to reduce symptom scores and inflammatory biomarkers in Crohn’s disease patients, as per the Cochrane Database of Systematic Reviews. Rifaximin, a non-absorbable antibiotic, has been found efficient in maintaining remission in Crohn’s disease in randomized controlled trials.
Despite the benefits, there are potential drawbacks and risks associated with the use of antibiotics in IBD treatment. Overuse of antibiotics can lead to further dysbiosis, antibiotic-resistant bacterial infections, and more severe Clostridium Difficile infections, thus counteracting the desired effects of antibiotics on disease activity.
Additionally, patients may experience adverse effects like nausea, peripheral neuropathy (nerve damage causing weakness or pain), and antibiotic-induced rash, which occur more frequently with metronidazole. Drug-drug interactions may also significantly limit the use of antibiotics, especially in patients who are already receiving multiple treatments for their IBD.
It is crucial to discuss with a healthcare provider before initiating antibiotic therapy for IBD, as the balance between benefits and risks is complex and significantly varies across individuals.
Antibiotics should be used as part of a broader, holistic approach to treating IBD, alongside dietary modifications, lifestyle changes, and other medications as necessary. This calls for personalized healthcare, optimizing therapy beneficiary effects, and minimizing associated risks.
Understanding the role of antibiotics in the treatment and management of Inflammatory Bowel Disease (IBD) requires keeping abreast of scientific research as it continuously evolves. Armoring yourself with knowledge is critical if you, or someone you know, are affected by IBD.

Patient Considerations and Doctor’s Advice
Contemplating the Use of Antibiotics in IBD
Inflammatory bowel disease (IBD) covers a host of conditions typified by persistent inflammation within the digestive tract. This includes diseases like Crohn’s disease and ulcerative colitis. The way these diseases present themselves can vastly differ between patients – producing a multitude of different symptoms. One potential treatment option is the use of antibiotic therapy which can be instrumental in the proficient management of IBD.
The exact etiology of IBD has not yet been definitively identified. However, it is widely accepted that gut bacteria and the human immune response contribute significantly to the development of these diseases and perhaps the induction of inflammation as well.
Antibiotics are believed to mitigate these effects by modifying the gut bacterial environment and reducing intestinal inflammation.
Therefore, they are viewed as a probable aid in the handling of IBD. However, before selecting this course of action, it is vital both for patients and their doctors to weigh the potential benefits against the factors to be considered during treatment.
Timing and Duration of Medication
The exact timing and duration of antibiotic therapy in managing IBD need to be carefully considered. The therapeutic aim is to achieve remission (absence of symptoms) while preventing the uncomfortable and potentially dangerous effects of recurrence.
For best results, your healthcare practitioner will tailor the regimen based on the severity of your condition and your body’s response to the medication.
The period during which antibiotics are taken will also depend on other factors that may be present, such as infections and abscesses, in which case the use of antibiotics may need to be extended. Ensuring you take the medication exactly as advised by your healthcare professional is essential to maintain the required level in your system and ensure the effectiveness of the treatment.
Possible Side-effects
Though potentially essential for relief and recovery, antibiotics may come with associated side effects, which can include nausea, diarrhea, or allergic reactions. Some antibiotics may also alter the delicate balance of your gut’s microbiome, leading to conditions such as Clostridium difficile infection.
Moreover, long-term use of certain antibiotics may cause resistance, diminishing their effectiveness over time. Therefore, healthcare professionals are cautious in prescribing extended periods of antibiotics unless it’s necessary, working closely with the patient to monitor the response to the therapy.
Interactions with other Medications
It is crucial to be aware that antibiotics may interact with other medications you are taking, potentially impacting their effectiveness or causing adverse effects. For instance, certain antibiotics can decrease the effectiveness of oral contraceptives. Always ensure that your healthcare professional is aware of all the medications and supplements you are currently taking.
Guidance of a Healthcare Professional
Perhaps, the most important aspect of antibiotic therapy for IBD is having the guidance of a healthcare professional to navigate through the complexities. Regular follow-ups and open communication play a pivotal role in adapting therapy to your body’s response, managing any potential side effects, and ensuring the effectiveness of the treatment.
Remember, antibiotics are powerful medicines, and while they can greatly improve the quality of life for many with IBD, they aren’t one-size-fits-all. It’s crucial to take them as directly recommended by your healthcare professional and to always discuss any concerns or changes in symptoms promptly.
In Conclusion
As we navigate the complex terrain of IBD and its management, the role of antibiotics proves to be a crucial element. Their multifaceted role, from reducing inflammation to addressing complications and maintaining balance in gut flora, is integral to a successful treatment plan.
However, it behooves both patients and healthcare professionals to remain conscious of potential side effects and contraindications associated with these treatments. Crucial here is the reminder that such medications should be taken solely under the guidance of a healthcare provider, tailoring treatments to individual needs and situations. As our understanding of IBD evolves, so too does our appreciation of the nuanced role that antibiotics can play in enhancing overall patient well-being and quality of life.


Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digestive enzymes Digestive Enzymes Supplement Digestive Health digital products Dr Sam Robbins Exercise Gut Health Gut Health While Travelling Health Tips for Travelling Healthy Living heart health HFL How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance Magnesium deficiency Matt Gallant mental health multivitamins Nootopia Nootropics Probiotics Probiotic Supplements reverse type 2 diabetes stress and anxiety stress relief vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea