Understanding Stress and Its Effects on IBD is a critical, but perhaps less understood, facet of living with this disease. The human body’s inherent ‘fight or flight’ response to stress can bring about a series of physical changes that may exacerbate IBD symptoms. As one delves into this matter, it becomes crucial to understand how IBD manifests, the complexity of stress, and the intricate ties that bind them.
Moreover, the myriad of ways that individuals with IBD can better manage stress and introduce lifestyle modifications to alleviate their condition is a subject of vast importance.
Understanding Stress and Its Effects on IBD
For those who suffer from chronic pain caused by IBD, it can not be overstated enough that any way to subdue this discomfort will be quite high on their list of priorities. The first thing many might think of is about dietary modifications and medication although managing stress is certainly something that IBD sufferers should pay attention to.
For one simply worrying and stressing about your health is not good anyway but from a physical point of view, the release of stress hormones such as cortisol in excessive amounts can itself worsen digestive health and IBD symptoms. Exactly, why this is so heavily recommended by doctors for patients with IBD.
Dealing with stress is important in so many ways and we will get back to this soon but for now…
What is IBD?
*Feel free to skip this section as I’m sure many will already know this information but anyhow so>>
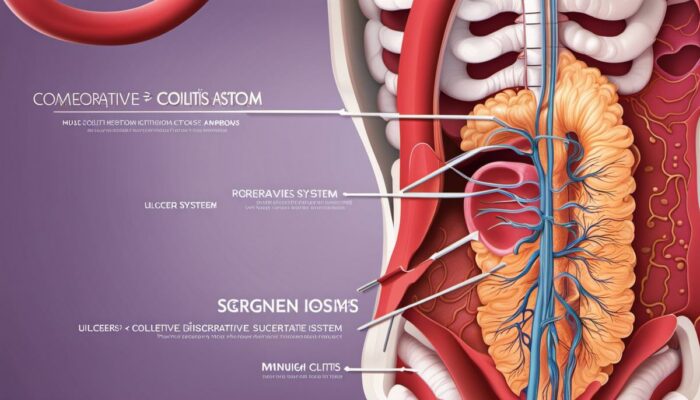
Inflammatory Bowel Disease (IBD), is an umbrella term for conditions characterized by chronic inflammation of the digestive tract, that can significantly impact the daily lives of suffering individuals. Ulcerative Colitis (UC) and Crohn’s Disease are the most prevalent types, causing debilitating symptoms that require intricate and often lifelong management.
Understanding Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease, commonly abbreviated as IBD, constitutes a group of intestinal disorders that cause prolonged inflammation in the digestive tract. The condition is categorized into two types – Ulcerative Colitis (UC) and Crohn’s Disease.
UC is primarily an ailment of the colon and rectum, where inflammation and ulceration occur in the innermost layer of the colon. Crohn’s Disease, however, is characterized by inflammation extending deep into the affected part of the digestive tract, potentially affecting various locations across the digestive system from mouth to anus.
IBD symptoms can range from mild to severe, fluctuating over time and differing from person to person. However, some common symptoms across the two primary IBD types include persistent diarrhea, abdominal pain and cramping, rectal bleeding, fatigue, and noticeable weight loss.
The prevalence of IBD globally is increasing, affecting millions of people and substantially reducing quality of life. Long-term effects of untreated IBD can extend beyond digestive issues to impact other body parts resulting in anemia, osteoporosis, liver disease, and even colorectal cancer.
Current treatments predominantly revolve around medication, lifestyle changes, and in more extreme cases, surgery, aimed at reducing inflammation and achieving disease remission.
Exploring the Impact of Stress on IBD
Chronic psychological stress is often associated with an increase in symptoms for those living with Inflammatory Bowel Disease (IBD), making it a substantial issue in managing the disease.
Whilst stress is not the cause of IBD, it can provoke a flare-up of symptoms and can prolong periods of disease activity. Essentially, the response to stress can increase intestinal permeability, alter gut movement, and change the functions of the gut’s nervous system – all of which can intensify IBD symptoms.
When faced with stress, the body produces a hormone called cortisol as part of its response mechanism. Over time, sustained high levels of cortisol may disrupt the body’s inflammatory response, which has the potential to exacerbate IBD symptoms and compromise the effectiveness of some IBD medications.
Methods of managing psychological stress, such as cognitive-behavioral therapies (CBT), relaxation techniques, regular physical exercise, along mind-body practices like meditation and yoga, are increasingly being recognized as vital complementary treatments for IBD.
While such practices may not directly cure IBD, they can contribute significantly to stress management, which in turn helps to mitigate the severity and frequency of symptoms, improve coping strategies, and enhance the overall quality of life for IBD patients.
In some circumstances, pharmaceutical interventions for stress, like anti-depressants and anti-anxiety medications, can also aid in stress management, but they must be considered on an individual basis due to potential additional side effects and drug interactions.

The Concept of Stress
Understanding the Nature of Stress
Stress refers to a physical and psychological reaction to situations that present demands on us or our environment that we perceive to exceed our current ability to handle or manage effectively.
The Body’s Fight or Flight Response
In response to stress, the body activates its ‘fight or flight’ response – a survival mechanism that prepares the body to deal with perceived threats. An increase in adrenaline and cortisol levels is observed, escalating heart rate and blood pressure, dilating pupils to enhance visibility, and mobilizing sugar and fat from storage reserves for instant energy.
While this response may prove beneficial in short bursts, frequently triggering it can precipitate a variety of health issues.
Different Sources of Stress
Stress can originate from an array of sources categorized into physical, emotional, and environmental categories. Physical stress may arise from ailments, bodily injuries, lack of sleep, or poor nutrition.
Emotional stress is typically tied to negative feelings such as anger, grief, or anxiety, possibly stemming from relationship issues, work pressure, or major life changes. Environmentally induced stress is associated with factors like pollution, noise, overcrowded spaces, or extreme weather conditions.
Chronic Stress and Overall Health
Continuous exposure to stressors can predispose an individual to chronic stress, where the body remains in a high-alert state for extended periods. Prolonged exposure to high cortisol levels (the primary stress hormone) can lead to deleterious effects such as poor sleep, lowered immunity, anxiety, depression, weight gain, memory impairment, and ultimately, an increased risk of heart disease.
Stress and Its Impact on Inflammatory Bowel Disease (IBD)
Stress has been empirically linked to the exacerbation of Inflammatory Bowel Disease (IBD), a condition characterized by chronic inflammation of the digestive tract. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, enhancing pro-inflammatory cytokine production that can inflame the gut.
This activation, coupled with the impairment of the natural barrier function of the gut, can precipitate IBD flares. Moreover, IBD patients frequently report that episodes of acute stress precede flare-ups of their symptoms, suggesting a profound interplay between the mind and gut, often referred to as the gut-brain axis.
This idea is further substantiated by research suggesting that stress management techniques, such as mindfulness-based therapy or yoga, may reduce the severity of symptoms and improve the quality of life for IBD patients.
Chronic stress appears to have a substantial effect on the prognosis of Inflammatory Bowel Disease (IBD). It may hasten the progression of the disease and potentially escalate the likelihood of surgical intervention.
It stands to reason that appreciating the significant role of stress in IBD could provide a more effective management approach.

The Connection Between Stress and IBD
Delineating Stress and IBD
Inflammatory bowel disease (IBD) encompasses conditions like ulcerative colitis and Crohn’s disease, commonly punctuated by alternating periods of remission and relapse. Manifestations of IBD may vary from abdominal discomfort and diarrhea to potentially fatal complications.
Notably, a significant number of individuals with IBD report that periods of psychological stress can exacerbate their existing symptoms or even trigger new ones.
Role of Stress Hormones
The body responds to stress by releasing hormones such as cortisol, adrenaline, and norepinephrine. This hormonal response prompts the ‘fight or flight’ response – an evolutionary mechanism designed to enhance survival. However, prolonged chronic stress exposure can lead to constant activation of these stress hormones, which can have harmful implications on various bodily systems, including the digestive system.
In the context of IBD, cortisol, in particular, is of significant interest. It not only reduces inflammation – a key feature of IBD – but also impacts the functioning of the gastrointestinal (GI) tract in numerous ways.
It suppresses the immune system, thereby potentially exacerbating IBD.
The Gut-Brain-Axis and Stress
Research on the connection between the gut and the brain has gained a lot of attention. The gut-brain axis signifies the reciprocal communication between the gut and the brain. The gastrointestinal tract is sensitive to emotion; feelings such as anger, anxiety, sadness, and happiness can all trigger symptoms in the gut.
Stress can alter gut physiology leading to changes in motility, increases in visceral perception, and changes in GI secretions. In individuals with IBD, stress has been shown to cause exaggerated responses from the gut, thus potentially increasing the severity of symptoms.
Studies Suggesting a Link
Numerous studies have been conducted focusing on the potential relationship between stress and the onset or worsening of IBD symptoms. In a review of 11 studies involving more than 2000 patients, Bitton et al. (2003) concluded that stress increased the likelihood of a flare-up in those with IBD.
Another study by Mawdsley and Rampton (2005) analyzed how psychological stress influences the disease course in IBD. It concluded that psychological stress could exacerbate IBD symptoms, suggesting that stress management should be an integral part of disease management.
Addressing Stress in IBD Management
Recognizing the possible influence of stress in IBD, it’s crucial to incorporate stress management techniques into treatment plans. Methods such as relaxation exercises, yoga, counseling, and cognitive-behavioral techniques have been found to be successful in reducing stress levels.
Particularly, some individuals with IBD have reported less severe symptoms when they have successfully managed their stress levels.
A deep understanding of the role stress plays in IBD could potentially lead to new treatment strategies. Besides, it could improve patient’s well-being, resilience, and overall life quality. Despite stress being an inevitable aspect of life, ensuring effective stress management strategies could substantially contribute to a more favorable disease course for IBD patients.
Dealing with Stress Whilst Living with IBD
The Link between Stress and IBD Explained
Inflammatory Bowel Disease (IBD) involves a collection of disorders that impact the gastrointestinal (GI) tract, namely Crohn’s disease and ulcerative colitis. Stress factors into the equation as it typically exacerbates or triggers flare-ups of these chronic conditions.
This is predominantly attributed to the gut-brain axis, a two-way communication system that connects the central nervous system with the enteric system (also known as the gut). During periods of stress, the body responds in a way that can aggravate the gut, resulting in discomfort, pain, and other symptoms related to IBD.
Managing Stress While Living with IBD
Managing stress when living with IBD is challenging but important. Evidence shows that chronic stress might not only contribute to the onset of IBD but also exacerbate its symptoms once present. Therefore, keeping stress levels in check is crucial.
Relaxation Techniques
Relaxation techniques can prove valuable in managing stress. Practices such as deep breathing, progressive muscle relaxation, or guided imagery can calm the mind and relax the body, thus reducing the impact of stress on IBD. These tools have been found to soften flare-ups and boost the effectiveness of medication regimes for IBD patients.
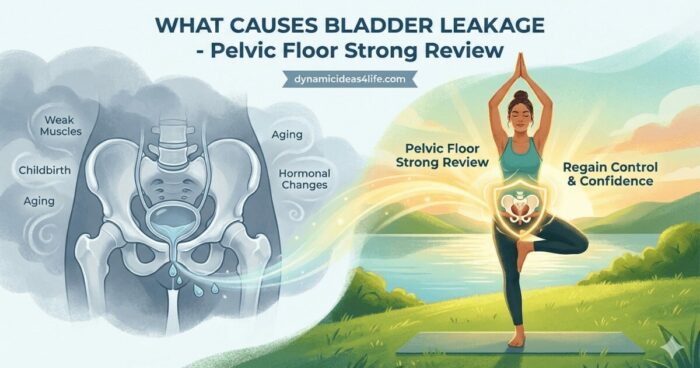
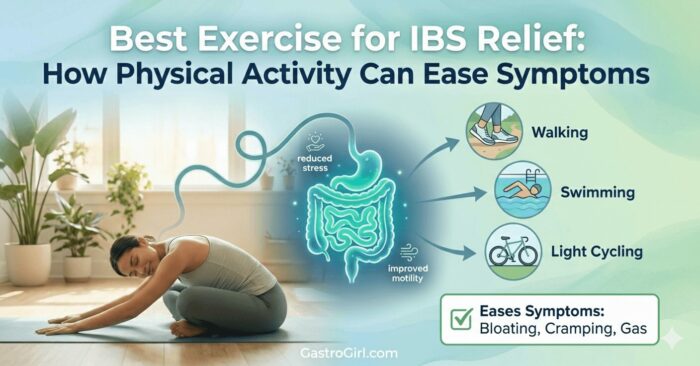
Regular Exercise
Regular exercise is another effective stress management tool. Evidence suggests that moderate physical activity can offset the negative effects of stress and reduce the risk of IBD flare-ups. Walking, cycling, swimming, or any other form of regular, moderate exercise can release endorphins, improve mood, and promote better sleep, all of which contribute to stress reduction and better symptom management.
Meditation
Meditation, especially mindfulness-based stress reduction (MBSR), has been found particularly effective in managing stress and improving the overall well-being of those living with IBD. MBSR teaches you to pay attention to your feelings, thoughts, and physical sensations without judgment.
This increased awareness can help you manage stress and mitigate the cycle of stress and symptom flare-ups characteristic of IBD.
Seeking Professional Support
If stress becomes overwhelming, seeking professional support is instructive. Psychologists, social workers, and psychiatrists are skilled in helping individuals manage stress through cognitive-behavioral therapy (CBT) or other therapeutic techniques.
Support groups, both online and in-person, may also prove beneficial. Sharing experiences with others who are facing similar challenges helps mitigate feelings of isolation, provides practical insights, and offers emotional support.
Stress and Lifestyle Balance in the context of IBD
Maintaining a balanced lifestyle is key to mitigating the effects of stress and its impacts on Inflammatory Bowel Disease (IBD). Ensuring regularity in meals, appropriate hydration, optimal sleep and evading triggers such as caffeine and alcohol can all assist in reducing stress levels.
This approach not only improves the management of symptoms but also enhances the overall life quality of an individual living with IBD.

Lifestyle Modifications to Ease IBD
Dietary Adjustments to Alleviate IBD
For those diagnosed with Inflammatory Bowel Disease (IBD), which includes conditions such as Crohn’s disease and ulcerative colitis, embracing a balanced diet is paramount. The body requires essential nutrients, vitamins, and minerals to operate accurately and to maintain the immune system.
However, during periods of flare-ups, dietary modifications may be required to lower the risk of symptom triggers. The influence of certain food types on IBD symptoms varies from person to person – some foods may worsen one’s symptoms, while others might have no effect.
Therefore, maintaining a food diary to note down possible trigger foods and subsequently eliminating them from intake is beneficial.
High-fiber foodstuffs, encompassing raw fruits, vegetables, and whole grains, have the potential to exacerbate symptoms during flare-ups and are therefore typically suggested to abstain from during these times. The inclusion of an abundance of lean protein, low-fiber carbohydrates, and healthy fats during meal planning is recommended.
Digestion can be eased if smaller and more frequent meals are opted for. Vitamin and mineral supplements may be necessary for individuals with IBD to cover any deficiency. To develop a custom-made dietary plan that caters to their specific requirements, consultation with a certified dietitian is advised for people with IBD.
Quitting Smoking and Moderation in Alcohol
Both smoking and excessive alcohol consumption serve as significant stressors to the body, exacerbating IBD symptoms. Multiple studies suggest that smoking makes Crohn’s disease more severe, whereas moderate drinking appears linked with a modest increase in relapse rates in ulcerative colitis.
Those with IBD should aim to quit smoking outright, and those who consume alcohol should do so in moderation. Again, moderation varies between individuals – what is tolerable for one person may trigger symptoms in another.
Abstaining from both smoking and excessive drinking can significantly mitigate IBD symptoms and improve a person’s overall health.
Approaches to Eating
Managing stress is key to managing IBD symptoms, and this extends to eating habits. Rushed meals or eating while stressed can exacerbate IBD symptoms. Techniques such as slow eating and mindful eating can significantly impact the digestion process.
Taking the time to eat well-cooked meals in a quiet, relaxed environment may help mitigate flare-ups by promoting better digestion and ideal nutrient absorption. Consuming foods at a comfortable temperature without rushing and chewing thoroughly can aid this process.
People with IBD are advised to drink lots of water but minimize consumption during meals, as it can dilute stomach acids and hamper digestion.
Physical Activity
Regular physical activity can play an essential role in managing the symptoms of IBD. Not only does exercise help to maintain physical health and well-being, but it also provides an outlet for stress and tension and aids in better sleep.
Low-impact exercises such as walking, swimming, yoga, and Pilates are excellent options. They do not place significant stress on the body while still promoting cardiovascular health and muscular strength.
Consult with a healthcare provider before starting any new exercise regime to ensure it is safe and suitable.
It’s important to note that managing stress goes hand-in-hand with these modifications. Combining these lifestyle changes with stress management techniques such as deep breathing, progressive muscle relaxation, mindfulness, meditation, and counseling can greatly ease the physical and emotional burden of IBD.
A holistic approach including dietary changes, physical activity, smoking cessation, moderation in alcohol intake, and stress management can significantly improve the quality of life of those with IBD making handling flare-ups more manageable.

In Conclusion
Paving the way towards improving the lives of people with IBD involves a multitude of factors, chief among them being the proper management of stress and the introduction of potential lifestyle changes. Acknowledging the diverse sources of stress and the significant toll they can take on the body, particularly the digestive system, is a necessary capacity to harbor.
Equally important is developing coping mechanisms such as adopting relaxation techniques or engaging in physical activities.
Furthermore, certain alterations to diet and other lifestyle habits, like abstaining from smoking and moderating alcohol intake, can give individuals a significant advantage in managing IBD symptoms. While living with IBD poses substantial challenges, a comprehensive understanding of the condition, the impact of stress, and the adoption of beneficial lifestyle modifications offer encouraging prospects for individuals navigating their journey with this chronic illness.
To read more about managing IBS and IBD Click HERE and for more about Stress and Anxiety click HERE<<<


Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digital products Dr Sam Robbins Exercise Gut Health Healthy Living heart health HFL how to lower blood sugar levels How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance list Magnesium deficiency Matt Gallant mental health multivitamins Nootopia Nootropics nutrient supplements Probiotics Probiotic Supplements proteolytic enzymes reverse type 2 diabetes stress and anxiety stress relief Supplements vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea