Acquiring a profound understanding of Inflammatory Bowel Disease (IBD) is an essential step toward efficiently managing the condition and improving a patient’s quality of life. This debilitating disease, which primarily includes two types namely Crohn’s disease and ulcerative colitis, displays symptoms that are not only physically challenging but exert a significant impact on one’s daily routines and mental health.
By delving into the details of IBD including its diagnosis, treatment, and coping strategies, individuals can gain a more in-depth insight into this intricate condition that affects many across the globe.
Understanding Inflammatory Bowel Disease
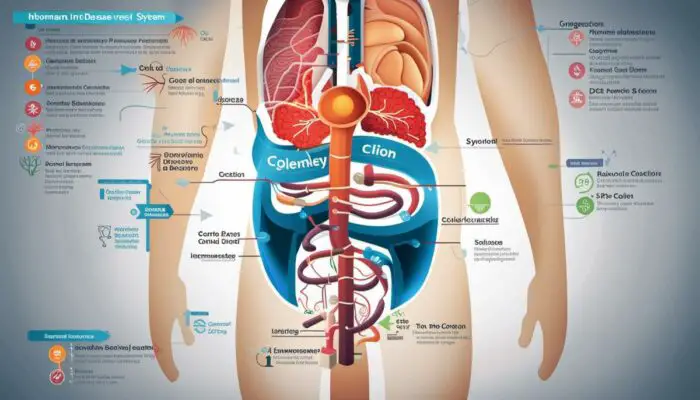
Inflammatory Bowel Disease (IBD) is an umbrella term used to describe disorders that involve chronic inflammation of the digestive tract. The inflammation can cause pain, severe diarrhea and may even lead to life-threatening complications. It is vital to recognize that IBD is not the same as Irritable Bowel Syndrome (IBS), which is a less severe condition that does not cause inflammation or damage to the bowels.
Types of Inflammatory Bowel Disease
The two most common types of Inflammatory Bowel Disease are Crohn’s Disease and Ulcerative Colitis. In essence, Crohn’s Disease can affect any part of the gastric tract from the mouth to the anus, causing inflammation deep within the tissue layers.
On the other hand, Ulcerative Colitis primarily targets the colon and the rectum, and it only involves inflammation in the innermost lining of the colon.
Both diseases manifest themselves with periods of relapse or flare-ups in which symptoms worsen and periods of remission when symptoms improve or disappear.
Recognizing Symptoms
Symptoms of IBD depend on the severity and location of inflammation. Common symptoms include;
- Prolonged Diarrhea,
- Rectal Bleeding,
- Abdominal Pain and Stomach Cramps,
- Reduced Appetite
- Unintended Weight Loss, and
- Fatigue.
More severe indicators may include fever, dehydration, rapid heartbeat, bloody stools, and in some cases, painful or frequent bowel movements.
Prevalence and Impact on Quality of Life
Approximately 3.1 Million adults (1.3%) in the USA live with IBD, equally affecting men and women. The disease prevalence has been increasing over recent years, possibly due to changes in environmental risk factors, although the exact cause is unknown.
The impact of IBD on quality of life is substantial. Not only does it cause physical discomfort and distress, but it also has a psychological impact, triggering feelings of anxiety, depression, and social isolation.
Fatigue, pain, and frequent need for the toilet can also limit daily activities and even affect employment or education. IBD is a very serious illness and it must be something that is prioritized.
Risk Factors for Developing IBD
The exact cause of Inflammatory Bowel Disease remains unknown, but several risk factors have been identified. These include age (most people are diagnosed before age 30, although the disease can onset at any age), family history, smoking habits, and use of non-steroidal anti-inflammatory medicines (NSAIDs).
Certain foods and stress do not cause IBD, but they can trigger symptoms in some individuals.
Also, there is a genetic predisposition to IBD, suggesting a hereditary component for these diseases.
Getting to Grips with Inflammatory Bowel Disease
Gaining a comprehensive understanding of Inflammatory Bowel Disease (IBD) is pivotal in raising public awareness, reducing societal stigma, and helping early diagnosis of this condition. With an enriched understanding of IBD, appropriate treatments can be identified and started promptly.

Diagnosis of Inflammatory Bowel Disease
Getting an accurate diagnosis for Inflammatory Bowel Disease (IBD) involves diverse procedures, each with the main goal of detecting signs of inflammation or damage within the digestive system. Health professionals typically kick-start this process with blood tests. This is a way for them to identify whether white blood cell count is elevated – a potential sign of inflammation.
On top of this, blood tests can highlight other key signs of IBD, such as anemia and reduced vitamin and mineral levels, which could suggest that the body is not properly absorbing nutrients.
Stool tests also play a vital role in the diagnostic process. They aid in determining if there’s unexplained bleeding in the digestive tract, indicative of IBD, and in eliminating other possible causes of the symptoms, like infections.
Note: You really should go to see a doctor if you believe you need a test to detect IBD but if this feels embarrassing or you can not fit this around work, or get a doctor’s appointment you can buy IBD Stool Tests online<<
*Findings of inflammation, such as heightened levels of proteins (calprotectin and lactoferrin) produced by white blood cells, equally suggest the potential presence of IBD.
Endoscopic Procedures and Imaging Studies
Patients may undergo endoscopic procedures for a more direct view of their digestive tract. Procedures such as colonoscopy or sigmoidoscopy involve inserting a thin, flexible tube equipped with a camera into the rectum, allowing doctors to closely examine parts of the digestive system.
A doctor may also take samples for further examination while performing these procedures.
For parts of the digestive tract not easily reached with a scope, imaging studies offer alternative methods of examination. These can include X-rays, CT scans, MRI scans, or capsule endoscopy using a camera pill that the patient swallows.
Such imaging studies provide comprehensive visuals of areas affected by IBD, including thickening of the intestinal wall, narrowing of the intestine, or issues with the surrounding tissues.
Use of Biopsies
Biopsy, extraction, and examination of tissue samples play an important role in diagnosing IBD. Taken during endoscopic procedures, biopsies can confirm inflammation and reveal the type of cells involved. Microscopic characteristics differentiate between the two main types of IBD, Crohn’s disease and ulcerative colitis.
Furthermore, biopsies help rule out other conditions that may have similar symptoms, like intestinal infections or colonic dysplasia, a precancerous condition.
Importance of Early Detection
Early detection of IBD is essential as it helps manage the disease effectively and mitigate potential complications, such as malnutrition, colon cancer, or holes in the colon.
Early treatment can also improve the quality of a patient’s life by reducing symptoms like abdominal pain, diarrhea, and fatigue. Therefore, understanding the symptoms and seeking immediate medical attention when symptoms persist is crucial.
Obstacles in IBD Diagnosis
Pinning down an exact diagnosis of Inflammatory Bowel Disease (IBD) can often prove complicated. Given the similar nature of symptoms presented by other gastrointestinal disorders, IBD can frequently be mistaken for conditions like Irritable Bowel Syndrome (IBS).
To compound matters, IBD symptoms can manifest in varying degrees of severity, making the diagnostic process even trickier. Hence, it is crucial to comprehend that typically, an accurate diagnosis of IBD involves a conglomerate of clinical, laboratory, endoscopic, and histopathological criteria.
Each diagnostic apparatus has its specification as well as limitation. For instance, IBD might not be definitively confirmed by just blood and stool tests.
Also, endoscopies might not be able to access certain parts of the digestive tract. Exactly why imaging studies may not accurately capture milder disease forms.
To add to the complexity, patient-related issues might also arise such as anxiety or reluctance to undertake specific procedures. However, despite drawbacks, these diagnostic techniques, when used in tandem with a detailed assessment of a patient’s medical history and symptoms, are indispensable to a comprehensive appraisal of IBD.

Treating Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) is a term encompassing a collection of conditions that result in inflammation of the digestive tract. The two most prevalent types are Crohn’s disease and ulcerative colitis. Chronic in nature, these diseases can cause substantial discomfort and significantly impair an individual’s quality of life.
Treatment Options for IBD
The primary goal of treating IBD is to reduce inflammation, manage symptoms, and achieve a long-term remission. Treatment options often involve a combination of medication, nutrition therapy, lifestyle changes, and sometimes surgery.
IBD Medication
Drug treatment is usually the first line of attack against IBD. The choice of medication depends on the severity of the disease, the patient’s overall health, and the side effects of the drugs.
Common types of medication used include anti-inflammatory drugs, such as aminosalicylates and corticosteroids, and immune system suppressors.
Biologic therapies are also used which target specific proteins in the body to reduce inflammation.
Side effects of these medications vary widely, from mild discomfort such as nausea, vomiting, and headaches, to more serious issues including an increased risk of infections due to immune system suppression.
Dietary Changes and Nutrition Therapy
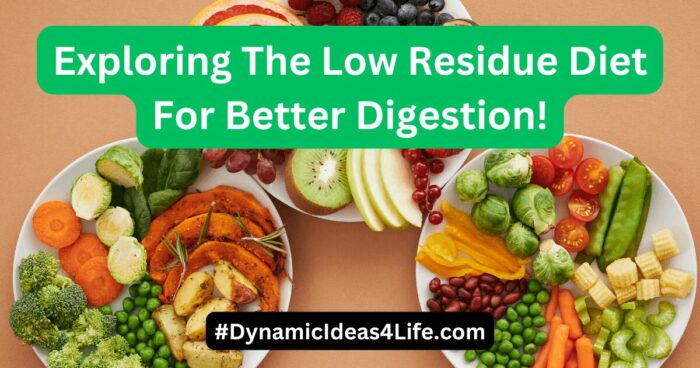
Living with IBD often means making adjustments to the diet. While there is no one-size-fits-all ‘IBD diet’, some general rules are to stay hydrated, eat smaller meals more often, and limit dairy products if they trigger symptoms. Nutrition therapy, such as special diets or the use of feeding tubes or nutrient-rich injections, may be necessary for individuals who are malnourished or experiencing severe symptoms.
Lifestyle Modifications
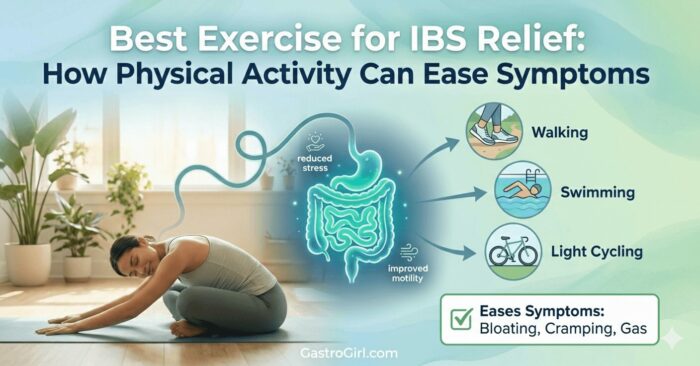
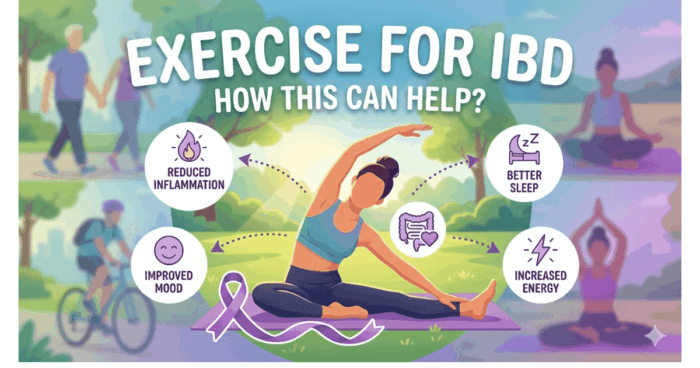
Smoking cessation is recommended, particularly for people with Crohn’s disease, as it can worsen the condition. Regular exercise can help manage symptoms by reducing stress and maintaining a healthy weight.
Mental health support, such as cognitive behavioral therapy or mindfulness practices, is also beneficial for managing the psychological stress associated with IBD.
Surgery for IBD Treatment
Surgery may be considered if diet, lifestyle modifications, and medicines haven’t been effective. For ulcerative colitis, surgery can usually “cure” the condition by removing the colon and rectum. For Crohn’s disease, surgery can provide some relief but is less likely to be a permanent solution as the condition often recurs. As with all surgical procedures, there are risks involved, which need to be weighed against the benefits.
The Role of the Patient
Patient empowerment is central to managing IBD. This means being informed about the disease, being proactive in seeking treatment and adjusting lifestyle habits, actively participating in clinical decisions, and staying up-to-date with scheduled screenings and doctor’s appointments.
Consequently…
IBD, such as Crohn’s disease or Ulcerative Colitis, entails a multifaceted management strategy that focuses on medication, dietary and lifestyle modifications, and sometimes surgery. For the effective handling of this chronic disease, a bridge between the patient and healthcare professionals is fundamental.

Living with Inflammatory Bowel Disease
Living with Inflammatory Bowel Disease is not confined to only managing physical discomfort. It also demands an intimate understanding of what triggers your flare-ups, lifestyle changes to mitigate symptoms, and a proactive approach to maintaining mental health.
Dietary Considerations with IBD
Food plays a key role in managing IBD. Although no single diet is recommended for everyone, certain foods may trigger inflammation and other symptoms. Consuming a balanced diet, rich in fruit, vegetables, lean meats, and whole grains can benefit overall health and help manage symptoms.
It may also be beneficial to keep a food diary to help identify any specific food triggers. Avoiding these foods can reduce the frequency and severity of flare-ups.
Additionally, some individuals may benefit from small, frequent meals rather than three large ones.
Dealing with Flare-ups
Recognizing the signs of an IBD flare-up, such as increased frequency of bowel movements, stomach pain, or blood in stool, is vital. When a flare-up occurs, it’s important to rest your body and maintain hydration.
Over-the-counter and prescribed medications can be used to control inflammation and manage symptoms. It’s crucial to communicate with your healthcare provider during these times, as adjustments to your treatment may be needed.
Mental Health and IBD
Living with a chronic condition like IBD can take a toll on your mental health. Symptoms such as fatigue or pain can affect mood and overall well-being. It’s common for individuals with IBD to experience feelings of anxiety and depression. Mental health professionals, such as psychologists and psychiatrists, can provide support and management techniques. Support groups, both online and in person, can also offer a sense of community and understanding.
Community Support For IBD Sufferers
Finding a community of individuals who understand the challenges associated with IBD can be immensely helpful. Support groups can provide a platform for sharing experiences, exchanging advice, and fostering understanding. Charities and organizations such as Crohn’s and Colitis UK can provide valuable resources and community connections.
Living with IBD
Life with IBD might not be easy, but it’s important to remember that you’re not alone. Many people have found ways to manage their symptoms and live full and fulfilling lives with IBD. As James, a businessman from Leeds who was diagnosed with Crohn’s Disease 15 years ago says, “IBD has made me appreciate the good days more.
I learned to listen to my body, pay attention to my diet, and lean on my family and support group when things get tough. It’s not a life sentence, it’s just a different way of living.”
Knowledge and Understanding of IBD
Knowledge and understanding of the condition, coupled with the right medical and emotional support, can go a long way toward managing IBD effectively. It’s about finding what works best for you, and feeling in control even when living with a chronic condition.
Expert Tips
Experts frequently recommend regular exercise to help in managing IBD. Physical activity can not only boost overall health but also help reduce stress and improve mood. Although you should still consult your doctor before starting any exercise regimen.
Secondly, regular appointments with healthcare providers ensure that your treatment plan is working and can be adjusted as required.
And lastly, make sure to get regular screenings for associated conditions like colon cancer, as individuals with IBD have a higher risk.

In Conclusion
Comprehending the multifaceted aspects of Inflammatory Bowel Disease empowers individuals to handle the condition more effectively. Whether it’s a commitment to treatment plans, making necessary lifestyle alterations, or seeking support within communities, each decision plays a vital role in managing the disease.
Investing time to truly understand the diagnosis process, treatment options, and everyday coping mechanisms makes a significant difference and paves the way toward a more balanced life despite the challenges presented by IBD. {Read More of Our Article About IBD and IBD HERE<<]
Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digestive enzymes Digestive Enzymes Supplement Digestive Health digital products Dr Sam Robbins Exercise Gut Health Gut Health While Travelling Health Tips for Travelling Healthy Living heart health HFL How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance Magnesium deficiency Matt Gallant mental health multivitamins Nootopia Nootropics Probiotics Probiotic Supplements reverse type 2 diabetes stress and anxiety stress relief vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea