Exploring the maze of Inflammatory Bowel Disease (IBD) requires a nuanced understanding of its manifestation, symptoms, and types. As an umbrella term, IBD encompasses conditions such as Crohn’s disease and ulcerative colitis, substantially affecting the digestive system and, by extension, the quality of life.
The insidious nature of these diseases can often complicate diagnosis and treatment. However, a keen observation of one’s dietary intake can offer a unique perspective on symptom management.
Exactly why with a plethora of food items potentially contributing to or alleviating symptoms, diet plans for managing IBD form such an integral part.
In this post, we shall look at exactly this to help you decide which dietary adjustments will suit you best. Please keep reading if this is something that you feel will be beneficial. If you or any of your loved ones suffer from IBD we hope this information serves you well. Now…
Creating Effective Diet Plans for Managing IBD
Understanding What Inflammatory Bowel Disease (IBD) is, starts with comprehension of its basic definition. We have already gone over what this is but just to expand further…
IBD is a collective term for conditions that cause chronic inflammation in the digestive tract. It is an umbrella term for several inflammatory conditions that affect the colon and small intestine. Its main types include Crohn’s disease and ulcerative colitis.
The inflammation triggered by IBD can cause a cascade of effects in the body.
Crohn’s Disease
Crohn’s disease is a type of IBD known for its patchy areas of inflammation, which may occur anywhere along the digestive tract from the mouth to the anus. The inflammation extends deep into the tissues, causing ulcerations and other complications.
The common symptoms include abdominal pain and cramping, persistent diarrhea, fatigue, and weight loss. Advanced stages of Crohn’s disease may even result in life-threatening complications such as intestinal obstructions, fistulas, and malnutrition.
Ulcerative Colitis
In contrast to Crohn’s disease, ulcerative colitis mainly affects the colon and the rectum. The inflammation, in this case, is continuous rather than patchy, typically starting in the rectum and extending further up the colon. Frequent symptoms of ulcerative colitis are similar to Crohn’s and include abdominal discomfort, bloody stools, fatigue, and significant weight loss.
Waves of active disease followed by periods of remission are typical for both diseases.
Impact of IBD on Everyday Life and the Role of Diet
The symptoms of IBD can carry notable impacts on daily life, disrupting normal activities and significantly affecting quality of life. The disorder’s episodic nature can also make it challenging for individuals to plan their routine activities, given the unpredictability of flare-ups.
The role of diet in managing IBD cannot be overstated.
Certain food items may exacerbate symptoms, while others can alleviate flare-ups and promote healing. While everyone is different and what works for one person may not work for another, there are some common dietary guidelines for people with IBD.
A personalized eating plan, developed with the help of a dietitian, can be very beneficial.
This may involve eating smaller, more frequent meals rather than three large meals per day, and drinking plenty of fluids. Some people may find they can tolerate a low-residue diet particularly well, which involves eating foods that are low in fiber as these are easier to digest.
It’s generally advised to avoid fatty, greasy, or fried foods, as well as a high intake of caffeine and alcohol.
Nutrient-dense meals can help manage symptoms and aid in the body’s healing process.
This typically involves a balance of protein, complex carbohydrates, and healthy fats. High-protein foods such as lean meats, poultry, fish, and eggs are often recommended.
Some suggested complex carbohydrates include oatmeal, brown rice, and whole-grain bread, while healthy fats can be found in foods such as avocados, nuts, and seeds.
Appreciating the role of IBD and comprehending how it impacts everyday life forms a crucial part of successfully managing these conditions.
It is indeed fundamental to seek advice from accredited dietetic professionals to design an individualized dietary plan, one that meets your personal nutritional requirements while aiding in symptom control.

The Relationship Between Diet and IBD
Inflammatory Bowel Disease (IBD) encompasses a group of illnesses causing chronic inflammation in your digestive tract, most notably Crohn’s disease and ulcerative colitis. These conditions are theorized to be set off or exacerbated by certain types of foods, though the specificity of the relationship is not yet completely deciphered.
Emerging research implies that a diet high in refined sugars, saturated fats, or meat may amplify the occurrence and intensity of IBD flare-ups.
Conversely, dietary components like fiber are notably beneficial for maintaining gut health. They facilitate regular bowel movements and encourage the growth of beneficial bacteria in the colon, presenting significant benefits for managing IBD.
Furthermore, due to intestinal inflammation or as a side effect of medication, individuals with IBD often face nutritional deficiencies. Therefore, a varied and nutritious diet can combat these deficiencies, thus enhancing overall health and well-being.
Personalized Dietary Plans in Managing IBD
In the management of IBD, a personalized dietary approach that considers an individual’s unique needs, preferences, and responses to food is critical. This is because people with IBD can have different dietary triggers or sensitivities. Hence, working with a dietitian has become an essential part of managing IBD.
The dietitian assesses your normal eating habits, nutritional needs, particular symptoms, and even lifestyle factors such as exercise and stress. Using this information, they develop a personalized meal plan that ensures adequate nutrition while minimizing symptom flare-ups.
Regular reassessments and alterations are made depending on symptom progression, ensuring the plan remains effective and appropriate.
The concept of ‘trigger foods’ in IBD
Trigger foods in IBD are essentially those that worsen symptoms. These could be anything from dairy products and glutinous foods to spicy foods or even certain types of fruits and vegetables. Intolerance to these foods isn’t universal; it varies significantly from one patient to another.
While identifying these trigger foods can be challenging, many dietitians recommend using a food diary. In this, you note down everything you eat and any subsequent symptoms you experience, from abdominal cramping to changes in bowel habits.
This journal can help pinpoint specific foods that exacerbate symptoms. It’s beneficial to eliminate suspected trigger foods for a while and then reintroduce them one by one to determine which foods truly affect your IBD.
Studying the interaction between diet and IBD reveals its vital and complex nature. It highlights how dietary management plays a crucial part in controlling IBD symptoms and enhancing the quality of life for patients, whether this involves retaining nutrition balance or uncovering foods that trigger reactions.
Building an Effective IBD Diet Plan
Diet and IBD: Understanding the Significance
IBD, an abbreviation for Inflammatory Bowel Disease, refers to healthcare conditions that include Crohn’s disease and ulcerative colitis. Diet management for these conditions can be demanding due to individual variations in response to different food types. For example, our bodies may respond to the same food in different ways based on genetics and environmental triggers amongst others, which means there’s no universal diet plan for IBD.
Nonetheless, there are some general guidelines that can be beneficial when it comes to crafting diet strategies to control IBD symptoms. Particularly, a person with IBD should consider consuming nutrient-dense, low-fat, and easily digestible foods. The key is to maintain a balanced diet that reduces the chances of nutrient deficiencies and at the same time eases symptoms.
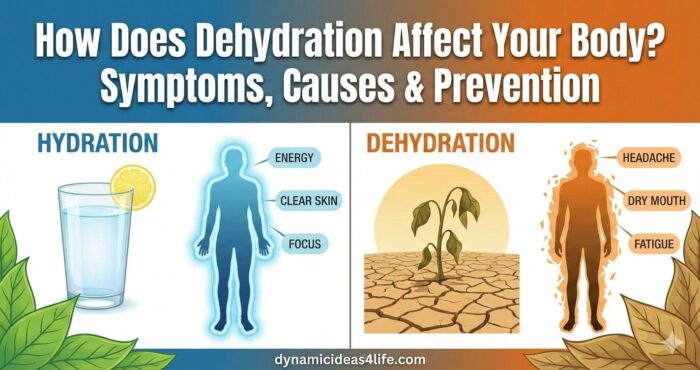
Hydration And IBD
Hydration is essential in an IBD diet plan due to the increased risk of dehydration from diarrhea – a common symptom among those with the condition. Besides water, electrolytes also need to be replaced, and drinks such as oral rehydration solutions or sports drinks can be included.
*My favorite tip here is to invest in a water purifier. Nothing beats pure and plastic-free drinking water. With mine, I like to add a couple of drops of apple cider vinegar for boosted nutrition.
Food Combinations And IBD
Some food combinations may be more beneficial than others for those with IBD. Foods high in soluble fiber, such as oats, can slow down the movement of food through the digestive tract and help reduce diarrhea.
It is better combined with lean protein sources such as chicken or turkey to avert triggering symptoms. Equally, easily digestible fruits and vegetables, along with starches like rice or potatoes, are mostly well-tolerated.
Meal Timings And Portion Sizes For IBD Diet
Frequent, smaller meals throughout the day instead of fewer, larger meals can help manage IBD symptoms as it’s lighter on the digestion process. Adopting this method can alleviate the overloading of the digestive system and reduce symptom flare-ups.
Proper portion sizes are crucial, as overeating can exacerbate the symptoms of IBD.
Professional Advice For Developing An IBD Diet Plan
Due to the individual nature of IBD, it is paramount to seek professional advice from dieticians and healthcare practitioners when planning a diet. Regular monitoring by healthcare professionals allows for necessary tweaks in the diet plan to control symptoms better, optimize nutrition intake, and enhance quality of life.
Alongside diet, it’s also important to consider other lifestyle variables like exercise, stress management, and rest for a well-rounded approach to managing IBD.
It’s essential to underscore that an IBD diet plan serves as an aid for managing symptoms, rather than a cure for the disease itself. Ensuring adherence to the prescribed medical procedures and maintaining a strong communication link with healthcare professionals will provide the best framework for managing this condition effectively.

Considerations and Precautions for Your IBD Diet Plan
Essential Aspects to Consider for an IBD Diet Plan
When dealing with inflammatory bowel disease (IBD), a term that covers conditions such as Crohn’s disease and ulcerative colitis, it’s vital to closely monitor dietary intake. The process of creating a personalized diet plan is greatly influenced by the severity and variety of the disease, as well as its impact on the specific individual’s digestive system.
It’s critical to note that certain foods may trigger a worsening of IBD symptoms. Nonetheless, because every individual is unique, these triggers differ from person to person, meaning a single diet cannot be universally recommended.
As such, a process of experimentation and observation is often necessary to figure out which foods help to control or provoke symptoms. Regardless of the specific foods included, a well-rounded diet comprising protein, whole grains, vegetables, and beneficial fats is crucial for supplying the necessary nutrients and promoting overall well-being.
Potential Nutritional Deficiencies
One significant concern for people with IBD is the risk of nutritional deficiencies. The inflammation and damage in the gut can lead to malabsorption of essential nutrients. For instance, deficiencies in iron, vitamin B12, calcium, and vitamin D are common, leading to anemia, fatigue, bone weakness, and other health issues.
To combat this, the diet plan should incorporate nutrient-rich foods that are easy to digest. In some cases, nutrient supplements may be recommended, but this should always be discussed with a healthcare professional to ensure safe, effective use.
Monitoring of Symptoms
Continuous monitoring of symptoms is a crucial part of managing IBD. This encompasses noting changes in bowel movements, pain levels, or overall discomfort following intake of certain foods. A food diary can be a helpful tool to identify potential triggers and assess the efficacy of dietary changes.
Changes in Appetite
It’s not unusual for people with IBD to experience changes in their appetite, especially during flare-ups. While it’s essential to maintain sufficient calorie intake for energy and healing, it may be necessary to adjust portion sizes or meal frequency to accommodate these fluctuations.
Efforts should be made to consume high-nutrition foods that are easy on the digestive system during periods of reduced appetite.
Adjusting the Diet Plan
In terms of IBD, the dietary plan is never static and should be adjusted based on changing needs and symptoms. Tailoring nutritional requirements, minimizing symptom triggers, and satisfying personal taste preferences are vital aspects of an adaptable IBD diet plan.
Consulting Health Professionals
The importance of consulting healthcare professionals before making significant dietary changes cannot be overemphasized. A registered dietitian or nutritionist with experience in managing IBD can offer personalized advice and guide the development of a diet plan.
Moreover, regular consultations with a healthcare provider are crucial for monitoring disease progression, adjusting treatment if necessary, and managing any complications promptly.
To summarise, successful dietary management of IBD requires a personalized and flexible approach, careful monitoring of symptoms, and regular consultation with healthcare professionals.
While it can be challenging, with patience and professional guidance, it is possible to manage the condition successfully and lead a healthy, fulfilled life.

Photo by monstruoestudio on Unsplash
The journey towards an effective IBD management diet plan is far more than just identifying nutritious, low-fat, and easy-to-digest foods. Therefore, care must be taken to ensure adequate hydration, beneficial food combinations, and appropriate portion sizes, while avoiding potential ‘trigger foods’.
While food plays a significant role, the undercurrent remains in tailoring the diet plan to the individual’s needs, monitoring symptoms, and adjusting the plan accordingly.
As appealing as it may be to take full control of your diet, consulting with healthcare professionals and dieticians before making significant changes is paramount.
Their expertise and guidance, coupled with your understanding of your symptoms and your body’s response to certain foods, form the foundation of a successful diet plan tailored for IBD.
>>>If you would like to read more about IBS and IBD check out our other posts here<<



Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digestive enzymes Digestive Enzymes Supplement Digestive Health digital products Dr Sam Robbins Gut Health Gut Health While Travelling Health Tips for Travelling Healthy Living heart health HFL How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance Magnesium deficiency Matt Gallant mental health multivitamins Nootropics nutrient supplements Probiotics Probiotic Supplements proteolytic enzymes reverse type 2 diabetes stress and anxiety stress relief vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea