Delving into the realm of medical science and understanding complexities of diseases like Inflammatory Bowel Disease (IBD) can often be daunting. Making sense of the relevant facts, serving as an informant of what IBD represents, and its major influences, symptoms and the various interventions available are a lot to comprehend.
The role of Immunosuppressive Drugs for IBD is a good example of this, and for this purpose this article unfolds a comprehensive understanding about how these drugs function, their administration and the vital concerns associated with their use.
Backed by real-life narratives, this piece aspires to provide a relatable picture for individuals on this treatment path. For those seeking treatment for IBD and considering Immunosuppresive Drugs this guide should provide with the information you need to know.
If you or someone you know suffers from IBD then please keep reading and tell us what you think towards the end in the comments. We hope you can find this information helpful. Now, Let’s begin…
A Comprehensive Guide to Immunosuppressive Drugs for IBD – What You Might Like To Know
Table of Contents
ToggleConsidering that Inflammatory Bowel Disease (Inflammation) happens as an Immune response it makes sense that Immunosuppressive medications are given to IBD patients. Some medications include;
1.) Corticosteroids such as Prednisone and Budesonide: These medications are typically used for short periods during flare-ups rather than as a long-term treatment.
2.) Antimetabolites like Azathioprine (AZA) and Mercaptopurine (6-MP): Often used as maintenance therapy to keep the disease in remission. They work by interfering with the DNA of immune cells, slowing their growth and activity. Methotrexate is another antimetabolite used if other drugs have proven ineffective.
3.) Biologics: The latest development in IBD treatment. These genetically-engineered proteins target specific parts of the immune system that contribute to inflammation.
*Examples include Infliximab (Remicade) and Adalimumab (Humira).
Understanding Inflammatory Bowel Disease
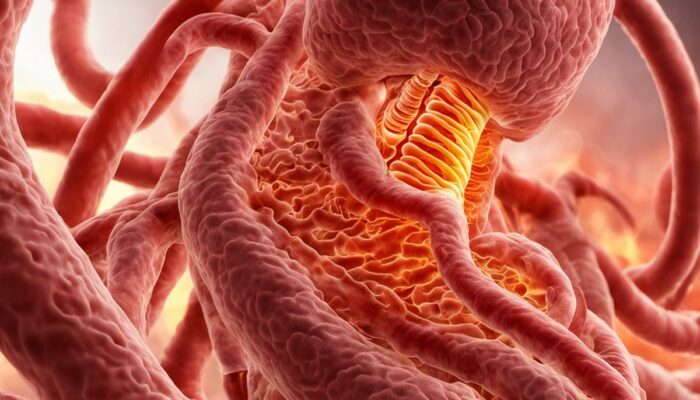
Inflammatory Bowel Disease (IBD) comprises a group of disorders that cause chronic inflammation in the digestive tract. The two main forms of IBD are Crohn’s Disease and Ulcerative Colitis. While Crohn’s can affect any part of the digestive tract, Ulcerative Colitis impacts the colon, also known as the large intestine.
The precise cause of IBD is unknown, but it is believed to result from an abnormal immune response, which could be triggered by genetics, environmental factors, or a mixture of both.
IBD symptoms might include persistent diarrhoea, abdominal pain and cramping, bloody stools, reduced appetite and weight loss. Acute flare-ups, marked by severe symptoms, are characteristic of the disease and can be extremely debilitating.
Treatment Options and Immunosuppressive Drugs
The primary aim of IBD treatment is to reduce inflammation, which can alleviate symptoms and potentially lead to long-term remission. Medications often come into play first. Although a variety of pharmaceutical classes can be used in the management of IBD, this piece will concentrate on immunosuppressive drugs.
Immunosuppressive drugs are medications that curtail the immune response. Given that IBD is caused by an overactive immune system that incorrectly attacks the cells in the digestive tract, immunosuppressants can help control this reaction and reduce inflammation.
Types of Immunosuppressive Drugs
The common types of immunosuppressive drugs used in treating IBD include corticosteroids, antimetabolites, and biologics.
Potential Side Effects and Risks
Although these drugs show considerable effectiveness, the administration of immunosuppressive drugs tends to carry with it a range of side effects. These can include an increased susceptibility to infections, along with cases of nausea, vomiting, and an elevated risk of certain types of cancer. To ensure effective management of these medications and their side effects, it is imperative to maintain rigorous patient monitoring.
It’s crucial to understand that while these drugs can significantly help manage symptoms and promote disease remission, by no means can they cure the condition. The management of IBD typically involves a multifaceted approach, coupling medication with lifestyle modifications such as alterations in diet, in addition to surgical procedures when required.
The aim of these combined strategies is to enhance the quality of life for patients living with these persistent conditions.
One must bear in mind that this information is a general overview and a discussion with healthcare professionals is always a necessity when it comes to individual treatment strategy.
What are Immunosuppressive Drugs?
Understanding Immunosuppressive Drugs
Immunosuppressive drugs constitute a class of medicaments explicitly constructed to reduce the body’s innate immune response. Under normal circumstances, the immune system acts as body’s defence against harmful entities, including but not limited to, viruses and bacteria.
Nonetheless, there can be instances where this system may react excessively or mistakenly target the body’s very own cells, resulting in an autoimmune disease. The function of immunosuppressive drugs, consequently, is to subdue this errant immune response.
Mechanism of Action
Immunosuppressive drugs can function in various ways to curb the immune system. Certain drugs work by inhibiting the synthesis of DNA in immune cells, thus reducing their proliferation. Other medications interfere with the activation or function of these immune cells.
In each case, the aim is to decrease an overly zealous immune response.
Typical Uses of Immunosuppressive Drugs
Immunosuppressive drugs are predominantly used in the prevention of organ transplant rejection, a process in which the recipient’s immune system identifies the new organ as foreign and attempts to destroy it. Another widespread use is in the treatment of autoimmune diseases.
In these scenarios, these drugs help to limit damage caused by the immune system attacking the body’s own cells mistakenly.
Immunosuppressive Drugs and IBD
Inflammatory bowel disease (IBD), such as Crohn’s disease and ulcerative colitis, is an example of an autoimmune condition that often involves an exaggerated immune response within the intestines. Immunosuppressive drugs have been particularly important and effective in the management of IBD.
They can limit inflammation in the gut and promote healing of the intestinal lining, thus reducing the severity of symptoms and improving the quality of life for those affected. The choice of which immunosuppressive medication to use is often determined by the disease severity, the location of inflammation within the gut, and the individual’s overall health.
It’s important to recognize that while these medicines are effective in managing active inflammation and maintaining remission, they can also present certain side effects. The main one being an increased vulnerability to infections resulting from the dampened immune response.
Therefore, it’s crucial to be under careful medical supervision whilst taking these medications.

Common Immunosuppressive Drugs for IBD
A Closer Look at Immunosuppressive Drugs for IBD
Immunosuppressive medicines serve as a prevalent means of treatment for Inflammatory Bowel Disease (IBD), encompassing conditions such as Crohn’s disease and Ulcerative Colitis. The goal of these drugs is to decrease inflammation by regulating the immune response that frequently exacerbates these conditions.
There are variations concerning the active components used, but predominantly their role is to inhibit the body’s immune activity, thus offering respite from symptoms and possibly staving off flare-ups.
Common Types of Immunosuppressive Drugs
There are several types of immunosuppressive drugs typically prescribed for IBD, including Aminosalicylates, Corticosteroids, Immunomodulators, and Biologics.
- Aminosalicylates, such as Sulfasalazine and Mesalamine, are often first-line treatments for IBD as they work directly on the affected areas of the intestines.
- Corticosteroids, like Prednisone, are powerful anti-inflammatory drugs that can quickly control acute symptoms but are not recommended for long-term use due to their side effects.
- Immunomodulators, including Azathioprine, Methotrexate, and Ciclosporin, modify the immune system and may be used when other treatments prove ineffective.
- Biologics, like Infliximab and Adalimumab, are a newer class of drugs that target specific parts of the immune system.
Effectiveness of Immunosuppressive Drugs
The effectiveness of these drugs can vary considerably among individuals. Some may find significant relief from symptoms, while others may see little to no improvement. It often takes trial and error to find the most suitable medication for each person.
Potential Side Effects
While immunosuppressive drugs can provide significant relief to IBD sufferers, they also come with potential side effects. These can range from mild, such as nausea, vomiting, and diarrhea, to more severe issues like kidney and liver damage, bone thinning, increased risk of infection, and even lymphoma in rare cases.
As such, it is crucial to discuss these potential risks with a medical professional before beginning treatment.
Considerations When Using Immunosuppressive Medicines
The possible side effects of immunosuppressive drugs shouldn’t deter you from taking them, especially if there are plenty of precautions you can take to mitigate these risks. Having regular blood tests is vital for monitoring the liver and kidney functions, as well as keeping track of your blood cell count.
Key practices such as washing your hands regularly, staying away from those who are sick and ensuring your vaccinations are up-to-date can all help to significantly lower your chances of infection.
Furthermore, faithfully following the prescribed medication dosage and promptly informing your doctor about any change in symptoms can greatly assist in the successful management of IBD.
It’s also important to remember that some immunosuppressive medicines may not start working immediately but can take several weeks or even months before you see improvements. Therefore, maintaining the course and being patient are crucial when dealing with these kinds of medications.
Real Life Experiences
Navigating Life with IBD: The Role of Medication
Immunosuppressive drugs have been a lifeline for many people dealing with Inflammatory Bowel Disease (IBD), enabling them to manage their symptoms and live more comfortable, normal lives.
Let’s look at Sarah’s example. Sarah, a 32-year-old woman from Manchester with a Crohn’s Disease diagnosis, a type of IBD, was put on Azathioprine, an immunosuppressant, as part of her treatment regimen.
Sarah did face challenges in the initial months as she coped with side effects such as feeling nauseous and tired. Additionally, she had to make changes to her lifestyle which included tightened control over her diet and limiting alcohol consumption.
However, as time went on, Sarah saw noticeable improvements in her condition. The distressing cramps and frequent trips to the loo started to reduce significantly. While the medication wasn’t a complete cure, it made a world of difference in improving her day-to-day life.
Turning a New Leaf
Martin, a 50-year-old man living with Ulcerative Colitis in East Sussex, shares a different narrative with immunosuppressive drugs. As part of his therapeutic regime, he was introduced to the drug Methotrexate. Alarmingly, he initially faced some violent reactions to the drug including severe mouth sores and loss of appetite.
However, through a process of gradual acclimatization, and with supportive measures in place like dietary changes, mouth rinses, and additional vitamin supplements, Martin reported a marked decrease in the rate of his flare-ups. It may have been a rocky start, but the improvements in his health outcomes were undeniable.
Everyday Hero
Then, there is the case of Emma, a lively teenager from Birmingham living with IBD. Diagnosed in her early teens, she was introduced to a combination of immunosuppressive drugs, including Mercaptopurine and Infliximab. Emma experienced initial challenges, particularly as she navigated the transition from child to adolescent amidst frequent hospital visits and educational disruptions.
Courageously, she embraced her condition, patient compliance being key to her success. Addressing her concerns of future fertility and long-term medication effects, her healthcare team reassured her, aiding in her overall journey. Emma engaged with online support groups, sharing experiences, and gaining comfort from those enduring similar battles.
A Tapestry of Individual Journeys
The personal experiences of patients managing Inflammatory Bowel Disease (IBD) using immunosuppressive drugs highlight a compelling truth; each journey is incredibly personal with effectiveness and side effects varying greatly.
Even with these challenges, a significant number of patients, much like Sarah, Martin, and Emma, have found these medications to be their saving grace. This mirrors the compelling reality that, despite initial hurdles and trials, a great many patients experience diminished symptom intensity, longer periods of remission, and fundamentally, an improved quality of life.

Future Advancements in IBD Treatment
Progress in the Medical Landscape for IBD
With the field of medicine constantly evolving, there are continuous advancements in the development of new immunosuppressive drugs and treatments, providing a beacon of hope for improved management of IBD. Moving beyond the traditionally used immunosuppressant drugs, such as corticosteroids, thiopurines, or cyclosporines, that work by suppressing the overall immune reaction, contemporary research now leans more towards identifying specific targets within the immune system.
The Emergence of Biologics
Biologics, products derived from living organisms, are being touted as the next wave in IBD treatment. They work by targeting specific components of the immune system rather than broadly suppressing the immune response. A new subtype of this group, known as anti-integrin therapy, essentially inhibits specific cell adhesion proteins (integrins) on the immune cell’s surface that allows it to travel to inflammation sites.
Vedolizumab, an anti-integrin, has shown significant promise in the treatment of IBD, specifically Crohn’s disease and ulcerative colitis.
Small Molecule Inhibitors
Another promising advancement in IBD therapy comes via ‘small molecule inhibitors’, such as JAK inhibitors. These drugs, which are usually taken orally, block specific pathways in the immune system’s signal transmission process called ‘Janus Kinase (JAK) pathways’, resulting in an immunosuppressive effect that mitigates inflammation. Tofacitinib, a JAK inhibitor, is currently in use for Ulcerative Colitis.
Personalised Medicine and Genetic Screening
There are future advancements in genetic profiling which might provide a more personalised way of treating IBD. Variations in the human genome might influence how someone responds to a drug, and genetic screening before treatment might become the norm for prescribing immunosuppressive drugs in future.
Stem Cell Therapy and Regenerative Medicine for IBD
There is also ongoing research into stem cell therapy and its use in regenerating damaged tissue in IBD patients. Autologous haematopoietic stem cell transplantation (aHSCT), where a patient’s own stem cells are used, has shown promise, and could be included in the therapeutic armamentarium for severe IBD cases that have been unresponsive to other treatments.
Future Challenges
While these advancements present hope for IBD sufferers, there are key challenges ahead that need to be addressed, such as the high cost of cutting-edge medications and therapies, and the limited accessibility to new treatments for patients in resource-poor settings.
The possibility of serious side effects and long-term impact of these novel treatments will also need to be evaluated and monitored over time.
Despite these hurdles, the overall trajectory of IBD treatment is gearing towards developing more targeted, personalized, safer, and more effective solutions. It is safe to say that the field of IBD research remains relentless in its pursuit of better treatment options, offering hope to patients across the globe.
In Conclusion
Despite the challenges associated with living and managing IBD, advancements in medical science are consistently striving towards a better future for everyone impacted. Continued research and development enable the discovery of new, improved treatment methodologies and medications, showing promise for a more effective management of this life-altering condition.
Throughout the sea changes in the medical field, one’s understanding of their body and disease coupled with an informed decision about treatment and medication can make all the difference. Sharing the triumphs and challenges of real patients serves as a reminder of human resilience and paints a real picture of life with IBD.
In this continuum of learning and evolving, may we also find the hope and strength to navigate these potentially turbulent waters with grace and dignity.
>>>If you would like to read more about IBS and IBD Relief<<<


Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digestive enzymes Digestive Enzymes Supplement Digestive Health digital products Dr Sam Robbins Exercise Gut Health Gut Health While Travelling Health Tips for Travelling Healthy Living heart health HFL How To Lower Cholesterol insulin resistance joint health supplement keto dieting Keto Diet Weight Loss leaky gut supplements list Magnesium deficiency Matt Gallant mental health multivitamins Nootopia Nootropics nutrient supplements Probiotics Probiotic Supplements reverse type 2 diabetes stress and anxiety stress relief vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea
About Author
Alex Chivers
Alex Chivers writes about natural health, nutrition, and lifestyle wellness at Dynamic Ideas 4 Life. His mission is to help readers discover practical, evidence-based ways to feel better, live healthier, and take control of their wellbeing — naturally.