At any given time, a significant proportion of the world’s population is Living with Inflammatory Bowel Disease (IBD), an illness that primarily affects the digestive system. It’s a mysterious and complex condition that can cause a great deal of discomfort and distress, yet is often misunderstood or overlooked.
In order to demystify this ailment, it’s essential to examine its nature, causes, symptoms, and diagnosis techniques. We will also delve into strategies to live with IBD, a variety of medical treatments available, and the significant impact this condition can have on one’s mental health.
This article seeks to provide a comprehensive understanding, shedding light on different facets of IBD to enable individuals to better manage their condition and maintain their quality of life.
Understanding IBD: Definition, Types, and Causes
Understanding IBD
Inflammatory Bowel Disease (IBD) is an umbrella term describing chronic inflammations of the digestive tract. IBD conditions are debilitating and characterized by relapses and remissions of the symptoms. The exact cause of IBD remains unknown, however, factors such as malfunction of the immune system and genetics are thought to play a significant role.
Environmental factors are believed to trigger the onset of the disease in a genetically predisposed individual.
Types of IBD: Crohn’s Disease and Ulcerative Colitis
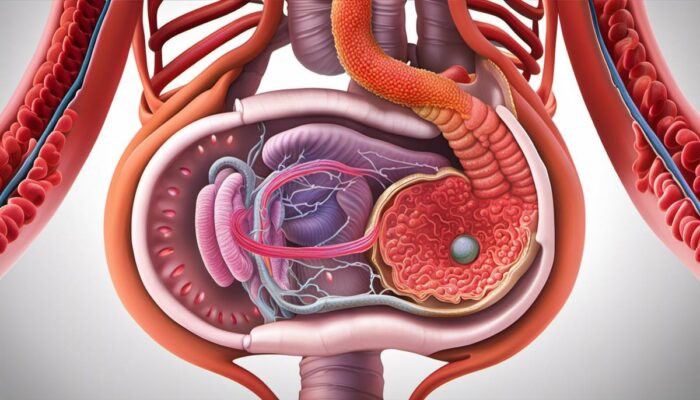
Primarily, there exist two types of IBD: Crohn’s disease and Ulcerative colitis. Both types manifest in the digestive tract and are distinct in terms of symptoms and area of effect.
Crohn’s Disease
Crohn’s disease can affect any part of your gastrointestinal tract, from the mouth to the anus. However, it often impacts the end segment of the small bowel (terminal ileum) and the beginning of the colon. In this condition, the inflammation involves the entire thickness of the bowel wall and the affected areas are interspersed between healthy ones.
Ulcerative Colitis
Ulcerative colitis, on the other hand, affects only the innermost lining of the colon (large intestine) and rectum. It usually begins at the rectum, extending upwards to a part or the entire colon. In this case, the inflammation occurs in a continuous stretch of the colon, unlike the interrupted pattern in Crohn’s disease.
Symptoms of IBD
Both conditions share symptoms including persistent diarrhea, abdominal pain, rectal bleeding, weight loss, and fatigue.
Probable Causes of IBD
While the precise causes of IBD are still under study, there are several factors hypothesized to contribute to its development.
- Firstly, there appears to be an irregular response of the immune system. Instead of fighting off harmful viruses or bacteria, the immune system attacks cells in the digestive tract, causing inflammation.
- Genetics also plays a significant role, seeing that IBD often runs in families. Scientists believe that certain genes that are inherited increase the risk of IBD.
- Lastly, environmental factors seem to play a part in the onset of IBD. Cigarette smoking, use of nonsteroidal anti-inflammatory medications, or a high-fat diet may increase the likelihood of developing these diseases.
In Summary
Becoming well-versed in the complexities of Inflammatory Bowel Disease (IBD) is an initial stride toward effectively managing and coexisting with this disorder. The medical community’s continuous efforts in research and the advancements in the field of science are revealing potential treatments that may cure or deter IBD in the future.
Symptoms and Diagnosis of IBD
Identifying the Symptoms of IBD
IBD, an abbreviation for Inflammatory Bowel Disease, is divided into two main types: Crohn’s disease and Ulcerative Colitis. Each of these conditions is characterized by persistent inflammation within the digestive tract, resulting in an array of debilitating symptoms that can significantly alter a person’s daily life.
The symptoms associated with IBD can diverge greatly between individuals and may change over time. Common symptoms, however, include constant stomach pain and cramping, diarrhea, rectal bleeding, excessive fatigue, substantial weight loss, and malnutrition owing to a loss of appetite and problems with absorbing nutrients.
People with Crohn’s disease may experience inflammation throughout their entire digestive tract, from the mouth right down to the anus. This widespread inflammation can result in persistent diarrhea, high temperatures, mouth sores, abscesses around the anal area, and inflammation affecting the skin, eyes, and joints.
Alternatively, Ulcerative Colitis predominantly affects the colon and rectum. People with this condition may experience symptoms such as bloody diarrhea, stomach pain, and cramping, an urgent need to defecate, and sometimes an inability to do so. Severe cases may result in additional symptoms like high temperatures, fatigue, dehydration, and unintentional weight loss.
Getting Diagnosed with IBD
Establishing a diagnosis for Inflammatory Bowel Disease (IBD) is often initiated with a thorough assessment of symptoms and a comprehensive study of one’s medical history. This is typically undertaken by a healthcare professional. Symptoms of IBD can be far-ranging and may mirror other medical conditions, making diagnosis both complex and time-consuming.
After a preliminary examination, additional tests may be required to affirm the diagnosis. These tests could include blood tests to measure inflammation levels and pinpoint any nutritional deficits, as well as stool tests for the detection of blood or any possible infection.
One prevalent diagnostic method is a colonoscopy, which permits doctors to examine the entire colon and rectum for signs of inflammation, bleeding, or ulcers. These visual markers can solidify the presence and severity of IBD.
Another investigation might include an endoscopy, inserting a camera in the digestive tract to inspect the inflammation’s scope and location. For a more detailed view of the gut, imaging tests like CT or MRI scans may also be utilized.
Where required, liver function tests may be conducted to scrutinize primary sclerosing cholangitis — a condition closely related to IBD, principally Ulcerative Colitis. This exhaustive diagnosis aids healthcare professionals in drafting an effective treatment plan specific to one’s signs and daily routines, ultimately helping to manage and lessen the symptoms of IBD.
The course of treatment typically incorporates medications, lifestyle modifications, and, occasionally, surgical intervention.
Living with IBD: Strategies and Tips
Modifying Diet when Living with IBD
Life with Inflammatory Bowel Disease (IBD) can often require significant modifications in the sufferer’s dietary patterns. As IBD impacts the digestive system, certain food items can escalate symptoms such as abdominal discomfort, bloating, or diarrhoea. Although there is no prescribed ‘IBD diet’, steering clear of certain foods may help manage the condition.
These typically include high-fiber foods (like fruits and vegetables), dairy products, spicy foods, caffeine,, and alcohol. It can also be beneficial to maintain a food diary, helping to identify foods that may trigger a flare-up of symptoms.
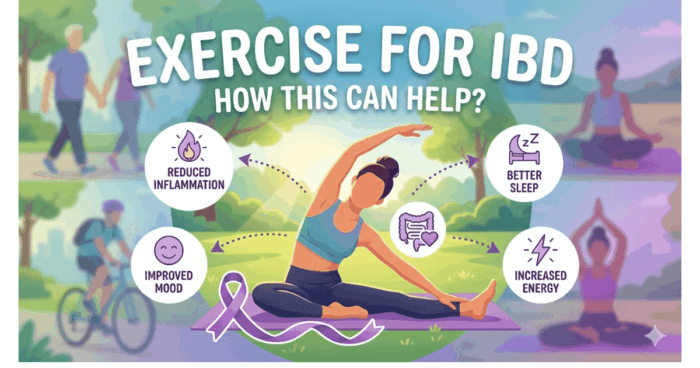
Physical Activity Recommendations
Physical activity can also play a critical role in managing IBD, despite popular belief. Regular exercise stimulates the body’s natural anti-inflammatory processes, reducing symptoms of IBD. It also has an important role in improving mood and reducing stress levels, which can indirectly contribute to symptom management.
Experts advise that individuals with IBD aim to undertake at least 30 minutes of moderate exercise most days of the week. This could include walking, swimming, cycling, or even gardening, depending on preference and comfort levels.
Stress Management Techniques
Psychological stress is recognized as a trigger for IBD flare-ups. Therefore, developing effective stress management techniques becomes an essential part of living with IBD. These strategies are unique to each person but could involve mindfulness training, meditation, yoga, deep-breathing exercises, or even simple leisure activities such as reading or listening to music.
Remember, the aim is to create a clear, calm mental space, reducing the likelihood of a stress-induced flare-up.
Regular Check-Ups
Regular check-ups are always advisable when living with IBD. Regular visits to a healthcare provider help in the early detection of flares and monitor disease progression. Diagnostic tests could become crucial in managing IBD proactively. Besides, open communication with healthcare providers allows for any concerns or changes in symptoms to be addressed promptly.
Medication and Treatment Adherence
While it may seem a no-brainer, it’s essential to stress the importance of sticking to the prescribed treatment plans. IBD medications are effective at controlling inflammation and maintaining remission, but only when taken correctly. Moreover, many medications require time to reach their full efficacy, and skipping doses can jeopardize this, resulting in more active disease and poorer outcomes.
Support Networks
Living with IBD can sometimes lead to feelings of isolation and emotional distress. Building and maintaining a robust support network is vital. Sharing experiences with others who understand what it’s like to live with IBD can help alleviate feelings of stress or distress.
Whether this network comes from family, friends, or local or online support groups, remembering that you’re not alone in the battle with IBD can provide an essential emotional bolster.
Living with Inflammatory Bowel Disease (IBD) calls for a multidimensional strategy that encompasses careful dietary planning, regular physical exercise, stress management, consistent medical check-ups, adherence to medication, and considerable support networks. Becoming skilled at managing each of these dimensions can significantly alleviate the challenges of living with IBD, ensuring you maintain the best possible quality of life.

Photo by brookelark on Unsplash
Medical Treatments and Medications for IBD
Grasping the Complexities of IBD
Inflammatory Bowel Disease is an umbrella term for a collection of intestinal conditions causing prolonged inflammation within the digestive system, encompassing both Crohn’s disease and ulcerative colitis. Common indicators of IBD can range from diarrhea, abdominal discomfort, and weight loss, to extreme tiredness.
Whilst the precise cause of IBD is yet to be discovered, effectively managing the symptoms and preventing flare-ups is essential. This necessitates comprehending the various available medical interventions, and potential risk factors, and adhering to guidelines to make well-informed decisions concerning your course of treatment.
Medications for IBD
Medication is often the first line of treatment for IBD. Physicians typically recommend anti-inflammatory drugs, the most common of which are Aminosalicylates. They are often used in treating ulcerative colitis or mild to moderate Crohn’s disease.
Corticosteroids, another type of anti-inflammatory medication, are used for more severe cases. However, they are not usually recommended for long-term use due to their side effects.
Immune system suppressors, like azathioprine or infliximab, work by reducing the body’s immune response. This not only alleviates inflammation but also reduces the chance of IBD flares.
Antibiotics may also be used if a patient has developed a fever or drainage due to an infection or if a fistula (an abnormal connection between different body parts) has developed.
IBD Surgery Options
In severe instances, surgery might become necessary. For ulcerative colitis, colectomy, the removal of the entire colon, is the primary surgical method. It is seen as a complete cure but can lead to significant changes in your daily life post-surgery.
In comparison, surgeries for Crohn’s disease like bowel resection or stricturoplasty, aim at relieving symptoms, but won’t cure the disease. Recurrence after surgery is common.
Innovative Therapies and Future Research Directions for IBD
Currently, several experimental treatments for IBD are being studied. Fecal microbiota transplantation (FMT), where stool from a healthy donor is transferred into the colon of a patient with IBD, is one experimental procedure that shows promise to help restore balance to the gut microbiome.
Stem cell transplants are also being investigated. The patient’s own stem cells are used to regrow the damaged portions of the intestine. While this research is still in the early stages, it offers potential hope for a long-term solution.
Similarly, dietary interventions, such as exclusion diets and prebiotics, are being explored as potentially effective ways of managing IBD.
Making Informed Decisions: Understanding Your IBD Risk Assessment
A critical part of managing life with Inflammatory Bowel Disease (IBD) is gaining an in-depth understanding of your condition and making informed decisions about your treatment. It’s crucial to be aware of the potential side effects that come with medications, including an elevated risk of infection and liver damage.
In addition to physical health considerations, you should also account for your emotional well-being. The lifestyle adjustments necessitated by a procedure like surgery may require you to seek further psychological support.
Arming yourself with knowledge can significantly help you in maneuvering through the complexities of living with IBD. Maintaining regular dialogues with your medical professional and conducting personal research can serve as pillars of strength that help in keeping you well-informed and ready for what lies ahead.
The Impact of IBD on Mental Health
The Unseen War: The Psychological Impact of Living with IBD
Inflammatory Bowel Disease (IBD) management reaches far beyond simply coping with physical symptoms like recurring stomach aches, diarrhea, and fatigue. The relentless struggle, hospital visits, and constant adjustments to life with a chronic illness can lead to profound impacts on a person’s mental health. Though sometimes understated, the importance of maintaining psychological wellness in managing this lifelong disease cannot be dismissed, making it a critical aspect it is necessary to draw attention to.
Recognizing the Psychological Impact
IBD doesn’t only affect the physical dimension of health. It’s also linked with increased levels of anxiety and depression. This can manifest in various forms. Individuals may live in constant fear of a sudden flare-up, leading to a state of perpetual anxiety.
Others may feel isolated or ostracised due to the nature of their symptoms, which can lead to feelings of depression. The uncertainty and unpredictability of this disease can also give rise to stress, and tension, and the sufferer may even experience body image issues due to weight changes or surgery scars.
It’s imperative to acknowledge these psychological struggles as part and parcel of the IBD journey.
Adopting Coping Strategies
Managing IBD’s mental toll requires strategies that encourage self-care and resilience. This can encompass a range of practices from mindfulness and meditation to regular exercise and maintaining a balanced diet. Patients are encouraged to keep a journal to document their emotions and feelings. This can often help pinpoint patterns in triggers or contribute to effective stress management.
Joining support groups, whether online or in-person, can also drastically change one’s outlook. Such groups offer an avenue to discuss fears and struggles with others who are going through the same experiences, enabling emotional support and nurturing a shared sense of community.
Seeking Professional Help
It’s not a sign of weakness to seek professional help, but rather a testament to the strength that it takes to confront the psychological aspects of living with this disease. Counseling, psychological therapies such as cognitive-behavioral therapy (CBT), or speaking to a psychiatrist can be enormously beneficial.
These mental health professionals can provide more structured support toward managing mood disorders linked to the disease and can offer coping mechanisms tailored to an individual’s unique needs and experiences.
Emphasizing a Holistic Approach
The road to managing IBD isn’t linear – it’s a continuous journey. Therefore, it’s crucial to take a holistic approach, integrating both mental and physical health concerns. IBD shouldn’t just be seen as a solely physical condition, but as an illness that has significant psychological aspects.
Nurturing the mind is as vital as treating the body in managing IBD, calling for greater emphasis on mental health support in patient care.
Coping mechanisms, quality psychological help, and empathetic support networks can all contribute to improving mental health outcomes for those with IBD.
Remember, it’s not just about living with IBD, it’s about living well with it.

The journey isn’t easy for individuals living with Inflammatory Bowel Disease, as it introduces an array of physical and emotional challenges to their lives. However, armed with accurate information about the disease, a toolkit of management strategies, and an understanding of available medical treatments, these hurdles can be navigated. Besides, acknowledging the mental health implications, developing resilience, and seeking psychological support when necessary will add a new perspective to managing this chronic disease.
In shining a light on these different elements of IBD, we hope that our readers feel more informed, empowered, and equipped to handle the curveballs that IBD may throw their way.



Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digestive enzymes Digestive Enzymes Supplement Digestive Health digital products Dr Sam Robbins Exercise Gut Health Gut Health While Travelling Health Tips for Travelling Healthy Living heart health HFL How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance Magnesium deficiency Matt Gallant mental health multivitamins Nootopia Nootropics Probiotics Probiotic Supplements reverse type 2 diabetes stress and anxiety stress relief vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea