How Does IBS Affect Mental Health? This might sound a little strange, how our thoughts can affect our physical health but how these two things are linked might surprise you. Indeed dealing with IBS can cause distress as well as discomfort but this goes a lot deeper. Understanding how the gut and brain work in unison together is just the tip of the iceberg.
The Gut-Brain Connection: How Does IBS Affect Mental Health?
The gut-brain connection refers to the bidirectional communication between the gut and the brain. It is a complex network of nerves, hormones, and chemicals that allows for constant communication between these two systems.
This connection is not only important for maintaining gut health but also plays a crucial role in mental health conditions such as anxiety, depression, and irritable bowel syndrome (IBS).
In this blog post, we will explore the various aspects of the gut-brain connection and its impact on mental health and IBS.
We will discuss the role of the gut microbiome in IBS and how imbalances in gut bacteria can influence mental health.
PLUS we will also delve into the relationship between stress and IBS, as well as the role of neurotransmitters and the vagus nerve in gut function and mental health.
Additionally, we will explore the psychological factors that can exacerbate IBS symptoms and the emotional toll of living with a chronic gut disorder.
And finally, we will discuss various treatment approaches and lifestyle modifications that can help improve the gut-brain connection and manage both IBS and mental health conditions.
The Role of the Gut Microbiome in IBS: How Bacteria Influence Mental Health
The gut microbiome refers to the trillions of bacteria that reside in our digestive tract. These bacteria play a crucial role in maintaining gut health by aiding digestion, producing essential nutrients, and supporting immune function.
However, research has shown that imbalances in the gut microbiome can have far-reaching effects beyond just gut health.
Several studies have linked imbalances in the gut microbiome to mental health conditions such as Stress, Anxiety, Depression, and IBS.
For example, a study published in the Journal of Gastroenterology found that individuals with IBS had significantly different gut microbiota compared to healthy controls. [R]
Another study published in the Journal Nature Communications found that certain gut bacteria can produce neurotransmitters such as serotonin, which is known to play a role in mood regulation. [R]
The exact mechanisms through which gut bacteria influence mental health and IBS symptoms are still being explored.
One theory is that imbalances in the gut microbiome can lead to increased intestinal permeability, also known as “leaky gut.” This can allow harmful substances to enter the bloodstream and trigger an immune response, leading to inflammation and potentially affecting brain function.
Additionally, certain gut bacteria can produce metabolites that can directly affect the brain and influence mood and behavior.
Stress and its Impact on IBS: Unraveling the Relationship between the Brain and the Gut
Stress has long been recognized as a trigger for IBS symptoms. Many individuals with IBS report that their symptoms worsen during times of stress or anxiety.
This relationship between stress and IBS symptoms is not surprising considering the close connection between the brain and the gut.
The brain-gut axis refers to the bidirectional communication between the brain and the gut.
The brain can influence gut function through the autonomic nervous system, which controls involuntary bodily functions such as digestion.
Stress activates the sympathetic nervous system, also known as the “fight or flight” response, which can lead to changes in gut motility, increased sensitivity to pain, and alterations in gut permeability.
Managing stress is crucial for individuals with IBS as it can help alleviate symptoms.
Stress management techniques such as deep breathing exercises, meditation, and yoga have been shown to be effective in reducing stress levels and improving IBS symptoms.
Additionally, cognitive-behavioral therapy (CBT) has been shown to be beneficial in managing both stress and IBS symptoms by helping individuals identify and change negative thought patterns and behaviors.
Neurotransmitters and IBS: Understanding the Chemical Messengers that Link Mental Health and Gut Disorders
Neurotransmitters are chemical messengers that transmit signals between nerve cells in the brain and throughout the body. They play a crucial role in regulating mood, behavior, and gut function. Imbalances in neurotransmitters have been implicated in both mental health conditions and gut disorders such as IBS.
Serotonin is one of the most well-known neurotransmitters and is often referred to as the “feel-good” neurotransmitter.
It is involved in regulating mood, appetite, and sleep. Research has shown that individuals with IBS may have lower levels of serotonin in their gut, which can contribute to symptoms such as abdominal pain, bloating, and altered bowel habits.
Other neurotransmitters such as dopamine and gamma-aminobutyric acid (GABA) have also been implicated in IBS.
Dopamine is involved in reward and motivation, while GABA is an inhibitory neurotransmitter that helps regulate anxiety and stress. Imbalances in these neurotransmitters can contribute to IBS symptoms and mental health conditions.
Targeting neurotransmitter imbalances in the treatment of IBS is an area of ongoing research. Medications that modulate serotonin levels, such as selective serotonin reuptake inhibitors (SSRIs), have shown some benefit in managing IBS symptoms.
However, more research is needed to fully understand the role of neurotransmitters in IBS and develop targeted therapies.
The Vagus Nerve, the Brain, and the Gut in IBS
The vagus nerve is a major component of the autonomic nervous system and plays a crucial role in the gut-brain connection.
It is the longest cranial nerve and connects the brain to various organs, including the heart, lungs, and digestive system.
The vagus nerve carries signals from the brain to the gut and vice versa, allowing for constant communication between these two systems.
It regulates various aspects of gut function, including motility, secretion of digestive enzymes, and inflammation.
Additionally, the vagus nerve is involved in regulating mood and stress responses.
Stimulating the vagus nerve has shown promise as a potential therapy for IBS and mental health conditions.
Vagus nerve stimulation (VNS) involves the use of a device that delivers electrical impulses to the vagus nerve, helping to regulate its activity.
VNS has been shown to reduce inflammation, improve gut function, and alleviate symptoms of depression and anxiety.
Psychological Factors in IBS Symptoms
The relationship between mental health conditions and IBS is bidirectional, meaning that they can influence and exacerbate each other. Individuals with IBS are more likely to experience anxiety and depression, and these psychological factors can worsen gut symptoms.
Anxiety and depression can lead to increased sensitivity to pain, which can amplify the perception of abdominal pain in individuals with IBS. Additionally, stress and negative emotions can trigger gut symptoms such as diarrhea or constipation.
The constant worry and fear of experiencing an IBS flare-up can also contribute to heightened anxiety levels.
Addressing mental health is crucial in the management of IBS. Cognitive-behavioral therapy (CBT) has been shown to be effective in reducing anxiety and depression in individuals with IBS.
CBT helps individuals identify and change negative thought patterns and behaviors that contribute to their psychological distress. Additionally, relaxation techniques such as deep breathing exercises and mindfulness meditation can help reduce stress levels and improve overall well-being.
The Impact of IBS on Mental Health: Exploring the Emotional Toll of Living with a Chronic Gut Disorder
Living with a chronic gut disorder like IBS can have a significant emotional and psychological impact on individuals. The unpredictable nature of IBS symptoms, such as abdominal pain, bloating, and altered bowel habits, can lead to chronic stress, anxiety, and depression.
Chronic pain is a common symptom of IBS and can have a profound effect on mental health. The constant discomfort and fear of experiencing pain can lead to feelings of frustration, helplessness, and even hopelessness.
Additionally, the embarrassment and social stigma associated with IBS can lead to social isolation and feelings of shame.
Addressing the emotional toll of living with IBS is essential for overall well-being. Seeking support from healthcare professionals, support groups, or therapy can provide individuals with the tools and resources to cope with the emotional challenges of living with a chronic gut disorder.
It is important to remember that individuals with IBS are not alone and that there are resources available to help them navigate their journey.
Treating IBS and Mental Health: Approaches to Addressing the Gut-Brain Connection
The treatment of IBS and mental health conditions requires a multidisciplinary approach that addresses both the physical and psychological aspects of these conditions.
It is important to recognize the interconnectedness of the gut and the brain and to develop treatment strategies that target the gut-brain connection.
Cognitive-behavioral therapy (CBT) is one approach that has shown promise in managing both IBS symptoms and mental health conditions. CBT helps individuals identify and change negative thought patterns and behaviors that contribute to their symptoms.
It can also provide individuals with coping mechanisms to manage stress, anxiety, and depression.
Gut-directed hypnotherapy is another treatment approach that focuses on improving gut function through relaxation techniques and visualization exercises.
This therapy has been shown to be effective in reducing pain, bloating, and other gut symptoms in individuals with IBS.
In some cases, medications may be prescribed to manage both IBS symptoms and mental health conditions.
For example, selective serotonin reuptake inhibitors (SSRIs) are commonly used to treat depression and anxiety and have shown some benefit in managing IBS symptoms.
Lifestyle Modifications for a Healthy Gut and Mind: Diet, Exercise, and Stress Management in IBS
In addition to medical treatments and therapy, lifestyle modifications can play a significant role in managing both IBS symptoms and mental health conditions.
Diet, exercise, and stress management techniques can help improve gut health and promote overall well-being.
Diet plays a crucial role in managing IBS symptoms. Certain foods can trigger gut symptoms such as bloating, gas, diarrhea, or constipation.
Keeping a food diary and identifying trigger foods can help individuals with IBS make informed dietary choices.
Additionally, following a low FODMAP diet, which restricts certain types of carbohydrates that can ferment in the gut, has been shown to be effective in reducing IBS symptoms.
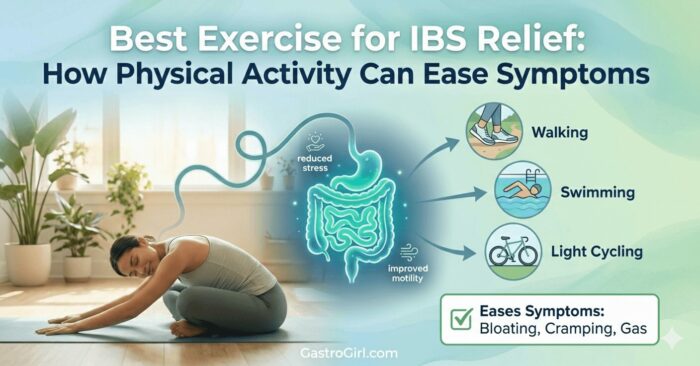
Regular exercise has numerous benefits for gut health and mental well-being. Exercise helps regulate gut motility and can alleviate symptoms such as constipation.
It also releases endorphins, which are natural mood boosters. Engaging in activities such as walking, jogging, yoga, or swimming can help reduce stress levels and improve overall well-being.
Stress management techniques such as deep breathing exercises, meditation, and mindfulness can help individuals with IBS manage stress levels and reduce the impact of stress on gut symptoms.
These techniques can be practiced daily or during times of increased stress or anxiety.
Research and Potential Therapies for Improving the Gut-Brain Connection in IBS and Mental Health
The understanding of the gut-brain connection and its implications for IBS and mental health is still evolving.
Ongoing research is focused on further unraveling the mechanisms through which the gut and the brain communicate and developing targeted therapies.
Potential future therapies for improving the gut-brain connection include probiotics, prebiotics, and fecal microbiota transplantation (FMT).
Probiotics are live bacteria that can help restore balance to the gut microbiome. Prebiotics are dietary fibers that serve as food for beneficial gut bacteria.
FMT involves the transfer of fecal matter from a healthy donor to an individual with a gut disorder, with the goal of restoring a healthy gut microbiome.
Other potential therapies include neuromodulation techniques such as transcranial magnetic stimulation (TMS) and transcutaneous vagus nerve stimulation (tVNS).
These techniques involve the use of non-invasive electrical or magnetic stimulation to modulate brain activity or stimulate the vagus nerve, respectively.
In Conclusion
In conclusion, the gut-brain connection plays a crucial role in both mental health and gut disorders such as IBS.
Imbalances in the gut microbiome, stress, neurotransmitters, the vagus nerve, and psychological factors can all contribute to the development and exacerbation of IBS symptoms and mental health conditions.
Understanding and addressing the gut-brain connection is essential for effective management and treatment.
A multidisciplinary approach that includes medical treatments, therapy, lifestyle modifications, and potential future therapies can help individuals with IBS and mental health conditions improve their quality of life and overall well-being.


Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digital products Dr Sam Robbins Exercise Gut Health Healthy Living heart health HFL how to lower blood sugar levels How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance list Magnesium deficiency Matt Gallant mental health multivitamins Nootopia Nootropics nutrient supplements Probiotics Probiotic Supplements proteolytic enzymes reverse type 2 diabetes stress and anxiety stress relief Supplements vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea