Within the labyrinth of our bodies reside the tales of health and illness. One such tale concerns Inflammatory Bowel Disease (IBD), which, while often silent and unassuming, holds significant implications for a person’s quality of life. Spanning from the mild discomfort of everyday life to severe and debilitating health events, IBD embodies a breathtakingly diverse range of experiences.
The twin branches of IBD, largely known as Crohn’s Disease and ulcerative colitis, have emerged as serious health concerns of our time. In our endeavor to shed light on these multifaceted conditions, we delve into a comprehensive exploration of IBD and the pivotal role played by colonoscopy in its detection.
By also equipping our readers with essential guidance on preparing for colonoscopy, our discourse aims to assuage any accompanying fears and uncertainties.
How Does a Colonoscopy Work For IBD Treatment?
Understanding Inflammatory Bowel Disease (IBD)
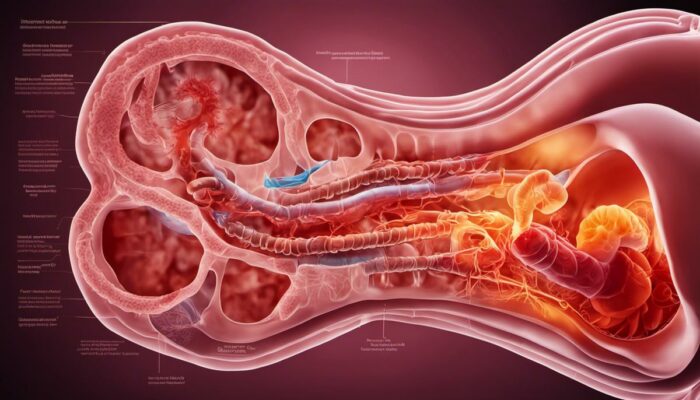
Inflammatory Bowel Disease, commonly known as IBD, is a term that refers to two main conditions characterized by chronic inflammation of the gastrointestinal (GI) tract, namely, Crohn’s disease and ulcerative colitis. These conditions can cause severe damage to the GI tract, disrupting normal bodily processes and thus, affecting the overall health of individuals.
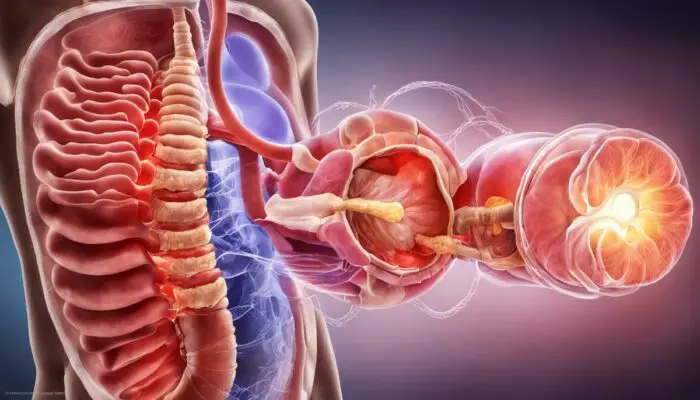
Crohn’s disease affects any section of the GI tract, from the mouth to the anus, potentially affecting each separate layer of the bowel walls. Ulcerative colitis, in contrast, impacts only the colon (the large intestine) which results in persistent inflammation and ulcers (sores) in the innermost lining of the colon and the rectum.
Interestingly, the ailments also differ in their flare-up patterns, with Crohn’s disease commonly demonstrating a ‘segmental’ pattern (healthy tissues interspersed with inflamed tissues) and Ulcerative colitis showing a ‘continuous’ pattern (consistently inflamed starting from the rectum and continuing upwards).
Symptoms of IBD
While both diseases are forms of IBD, they manifest different symptoms. However, some common symptoms across both include persistent diarrhea, rectal bleeding, abdominal pain, drastic weight loss, and fatigue.
With Crohn’s disease, symptoms can range from mild to severe and may develop gradually over time or could even come on suddenly without any warning.
Ulcerative colitis often starts with minor symptoms that gradually escalate over time, further progressing into severe bouts of bloody diarrhea, abdominal discomfort, and frequent need to evacuate the bowels.
Causes and Prevalence of IBD
The exact causes of IBD remain unclear, though it is widely acknowledged that these diseases are caused due to an overactive immune response triggered by various factors such as genetics, environment, and an imbalanced gut microbiome.
A family history of IBD increases the likelihood, suggesting a strong genetic component. Other factors such as a Western diet, smoking, and the use of nonsteroidal anti-inflammatory drugs (NSAID) are cited as contributors to the disease.
In terms of prevalence, IBD affects millions globally, with substantial increases in newly diagnosed cases, especially in developing countries. According to data from Crohn’s & Colitis UK, approximately 300,000 people are diagnosed with IBD across the UK.
Crucial Role of Colonoscopy in IBD Diagnosis and Management
Colonoscopy, a significant medical intervention, is a key method in diagnosing and managing Inflammatory Bowel Disease (IBD). During a colonoscopy, a long, bendable tube (termed a colonoscope) is carefully inserted into the rectum to examine the internal lining of the large intestine.
This procedure assists medical professionals in ascertaining the severity and reach of the inflammation present as well as the degree of ulceration. Crucially, it helps distinguish between Crohn’s Disease and Ulcerative Colitis, two forms of IBD that require different treatment.
Regular colonoscopies also support ongoing IBD management, enabling doctors to monitor disease progression, evaluate treatment effectiveness, and detect any complications early such as dysplasia or colorectal cancer. Despite any natural worry, it’s essential to recognize the significant part colonoscopy has in tackling IBD effectively.
The Role of Colonoscopy in Detecting IBD
Relevance of Colonoscopy in Detecting IBD
Colonoscopy substantially contributes to the initial detection and formal diagnosis of Inflammatory Bowel Disease (IBD), which includes conditions like Crohn’s Disease and Ulcerative Colitis. This key procedure not only plays a role in establishing if an individual is suffering from IBD but also in differentiating between the two key types of the disease. Despite presenting with similar symptoms, these disorders require distinct treatments, making the role of colonoscopy in accurate diagnosis invaluable.
How is a Colonoscopy Performed?
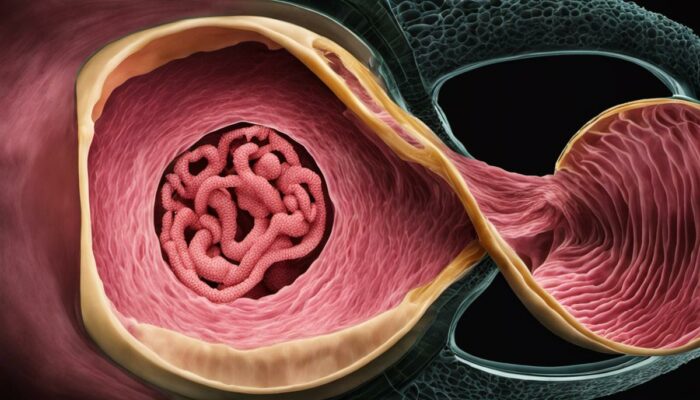
A colonoscopy is an endoscopic investigation of the large colon and the distal part of the small bowel using a small camera affixed to a long, flexible tube. This instrument called a colonoscope, is gently inserted into the anus and advanced through the rectum and into the large intestine.
This process allows for clear visualization of the entire colon and rectum. If required, small tissue samples can also be taken during the procedure for further examination, through a process called biopsy.
The procedure typically takes around 30 to 60 minutes and is conducted under sedation to make it as comfortable as possible for the patient. Certain dietary restrictions must be followed in the days leading to the procedure, and a clear liquid diet is recommended the day before.
A laxative solution or enema may also be prescribed to cleanse the colon, ensuring unobstructed observation.
What Does a Colonoscopy Detect?
A colonoscopy has the advantage of revealing early symptoms or indicators of IBD that may not yet be evident, thus potentially facilitating early diagnosis and treatment. It can identify redness, swelling, and sores on the lining of the intestines.
Polyps or growths can be detected and even removed during a colonoscopy, a critical step in preventing colon cancer.
In the case of IBD, a colonoscopy can be particularly needful, as it can reveal tell-tale signs such as areas of inflammation, ulceration, or bleeding. It can also help in assessing the severity of the inflammation, which is paramount in deciding the course of treatment.
Colonoscopy – A Vital Tool in IBD Diagnosis
When it comes to diagnosing Inflammatory Bowel Disease (IBD), a colonoscopy is often seen as the ‘gold standard’. This is largely due to its high sensitivity in detecting changes in the colon and negligible major side effects. A colonoscopy provides a detailed real-time view of the entire colon, allowing healthcare providers to assess the health of the bowel in great detail.
Of particular value is the ability to perform biopsies for further examination under the microscope. Combined with other diagnostic methods such as symptom analysis, laboratory tests, and radiological studies, a colonoscopy paints a comprehensive picture. This vital information empowers the healthcare team to develop a tailored and effective treatment program.
Preparing for a Colonoscopy
Exploring the Intricacies of IBD and Colonoscopy
IBD, or Inflammatory Bowel Disease, is an umbrella term for illnesses that result in long-lasting inflammation within the digestive tract. The most common manifestations are Crohn’s Disease and Ulcerative Colitis. Individuals with IBD may experience a variety of symptoms, such as frequent diarrhea, abdominal discomfort, overwhelming fatigue, visible blood in stools, and unexplained weight loss.
The diagnosis of IBD is mainly made using colonoscopy. This investigative procedure enables doctors to have a closer look at the large intestine, making it possible to detect inflammation, any signs of bleeding, or the presence of abnormal growths.
The Importance of Colonoscopy in IBD
For IBD patients, a colonoscopy is valuable in monitoring the state of the disease, gauging how well treatment plans are working, and determining whether it’s in remission or worsening. Furthermore, it’s crucial in detecting complications such as strictures, abscesses, or even colon cancer. As such, preparing accurately for a colonoscopy is essential to ensure accurate and helpful results.
Your Initial Preparation
In the days leading up to the procedure, you’ll need to adapt your diet to help thoroughly cleanse your colon. This usually involves switching to a low-fibre diet around 3 to 4 days before the colonoscopy, avoiding foods such as fruits, vegetables, beans, and whole grains. The day before the procedure, you’ll typically need to consume only clear liquids, like broth soup, black tea, clear juices, or jelly, staying clear of any foods or drinks that are red or purple in color.
Colon Cleansing
The most critical part of the preparation involves colon cleansing, normally performed with a prescribed laxative regimen, often called ‘bowel prep’. This is taken the day before and the day of the colonoscopy. Follow the instructions given by your medical team rigorously for this procedure, as an incompletely cleansed colon may cause the colonoscopy to be ineffective or require a repeat procedure.
Medication Considerations
Your healthcare provider should be aware of all medications you’re currently taking, as some may require adjustments before the colonoscopy. Blood thinners or certain diabetes medications, for instance, might need to be temporarily stopped. However, never stop or alter your medication routine without consulting your healthcare professional beforehand.
During the Colonoscopy
Complications during a colonoscopy are rare, though it’s reasonable to feel a bit anxious. You’ll be sedated and likely won’t remember much about the procedure. After sedation, a colonoscope – a long, flexible tube with a camera at the end – is gently inserted into your rectum and guided through your colon. You might feel some pressure or mild cramping during the procedure, but generally, any discomfort is minimal.
Biopsies and Polyp Removals
During a colonoscopy, biopsies (where a small sample of tissue is collected) may be taken without causing any pain. Similarly, polyps, which are abnormal growths in the colon, can be removed. This is important as some polyps can eventually develop into cancer if left in place. Again, this procedure is usually carried out painlessly.
Preparing for a colonoscopy holds substantial implications for your Inflammatory Bowel Disease (IBD) management efforts. Understanding what to expect, both during the preparation and procedure can greatly impact the success rate of the colonoscopy.
Ensuring this process goes smoothly provides your healthcare team with the best chance of effectively diagnosing, monitoring, and treating your condition.
Life with IBD: Management and Living a Normal Life
Grasping IBD and Its Influence
Inflammatory Bowel Disease includes various inflammatory conditions implicating the colon and small intestine. The most prevalent types, Crohn’s Disease and Ulcerative Colitis, can induce symptoms such as abdominal discomfort, intense diarrhea, fatigue, weight loss, and malnutrition. Managing IBD can be an arduous task given its chronic nature and the disruptive impact it can cause in daily life routines. Nevertheless, if managed appropriately, those affected by IBD can lead normal and fulfilling lives.
Managing IBD through Medication
The first line of treatment for IBD often involves prescription medication. Anti-inflammatory drugs, immunosuppressants, and biological therapies aim to reduce inflammation and manage symptoms. The type of medication prescribed will depend on the severity of symptoms and the type of IBD.
Importance of Regular Monitoring and Check-ups
Consistent monitoring of one’s health status is crucial when living with IBD. Regular doctor’s appointments and health check-ups are necessary to monitor the disease’s progression and the effectiveness of the treatment strategy. A colonoscopy, which is a procedure involving a long, flexible tube inserted rectally to view the entire colon lining, is all too familiar for those with IBD. It’s an essential tool in managing IBD as it can detect any changes or abnormalities early, enabling prompt and necessary adjustments in treatment.
Food and Nutrition
Nutrition significantly impacts IBD. Some foods can exacerbate symptoms, so it’s important to identify and avoid them. Keeping a food diary can assist in identifying these triggers. While it’s important not to restrict one’s diet unnecessarily, a well-balanced diet is imperative in providing the necessary nutrients needed to manage the disease and ensure overall well-being. In severe cases, a dietician might recommend special diets or nutritional supplements.
Keeping Active and Staying Positive
Regular exercise is beneficial for individuals with IBD. While the condition can sometimes make exercising difficult, low-impact activities such as walking, swimming, or yoga can help reduce stress, improve mood, and promote overall health.
Just as vital is maintaining a positive mindset. IBD can impact mental health, leading to stress, anxiety, and depression. Therefore, seeking mental health assistance such as counseling or joining support groups can be invaluable for emotional well-being.
Personal Care and Routine
Proper care and routine can’t be overstated when living with IBD. Having a regular sleep schedule aids in reducing stress and maintaining a healthy immune system which is crucial for disease management. Good personal hygiene, especially when administering medication, can prevent infection.
Lifestyle Modifications
Lifestyle modifications are often necessary for managing IBD. For instance, planning your day around easy access to restrooms or carrying spare clothes could be necessary measures. Likewise, adjusting work schedules or even work itself can help accommodate the urgent nature of the disease. It’s important to remember these adjustments aren’t hindrances but steps toward living a normal and productive life with IBD.
In Conclusion
As our journey through the world of IBD unfolds, we hope to arm our valued readers with essential insights into this complex condition. Through understanding comes empowerment, and we endeavor to equip every individual with the knowledge to navigate the labyrinth of IBD.
From acknowledging the fundamental role of colonoscopy in timely detection, shedding light on effective preparation, to the mastery of life amid the trials of this enduring condition, we aim to foster a community prepared to face IBD head-on. Remember, it’s not the challenges that define us, but rather, how we overcome them.
In facing IBD, knowledge is a beacon guiding us toward our shared goal: a healthier, brighter future for all.

Anxiety and Depression BiOptimizers blood pressure supplements blood sugar control blood sugar support supplements cognitive function digestive enzymes digital products Dr Sam Robbins Exercise Gut Health Gut Health While Travelling Health Tips for Travelling Healthy Living heart health HFL how to lower blood sugar levels How To Lower Cholesterol insulin resistance joint health supplement keto dieting Keto Diet Weight Loss leaky gut supplements list Magnesium deficiency Matt Gallant mental health multivitamins Nootopia Nootropics Probiotics Probiotic Supplements proteolytic enzymes reverse type 2 diabetes stress and anxiety stress relief Supplements vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea