For many who do not know How To Tell The Difference Between IBS and IBD this can seem a lot to wrap your head around. As the stresses and pace of modern life continue to escalate, a rising number of individuals are experiencing these digestive difficulties. These can lead to persistent and sometimes debilitating pain that could either be Irritable Bowel Syndrome (IBS) or Inflammatory Bowel Disease (IBD).
Yet, both of these disorders, while sharing similar symptoms, are fundamentally distinct in their causes, treatments and impact on individuals. This comprehensive guide explores an overview of both IBS and IBD, drawing from current research and medical knowledge.
Additionally, it delves into a detailed comparison and contrast between the two, to clarify common misconceptions and shed light on their key differences.
Furthermore, this guide contemplates the profound implications these conditions can have on a person’s daily life and proposes strategies for managing their symptoms effectively.
So let’s get started…
How To Tell the Difference Between IBS and IBD
I will of course look to answer this question more thoroughly as this post continues but for those looking for a short answer here is what is the commonly accepted view;
“The main way to tell between IBS and IBD is by the severity of the symptoms. For instance, if you have the typical discomfort of IBS with no resolution from bowel movements and you suffer from symptoms such as Anemia, bleeding, weight loss, and fever then this could indicate that you have IBD rather than IBS”.
There is certainly a bit more to it than this but this is the short answer. If you would like to know more then please keep reading on>>
Understanding What Is Irritable Bowel Syndrome (IBS)
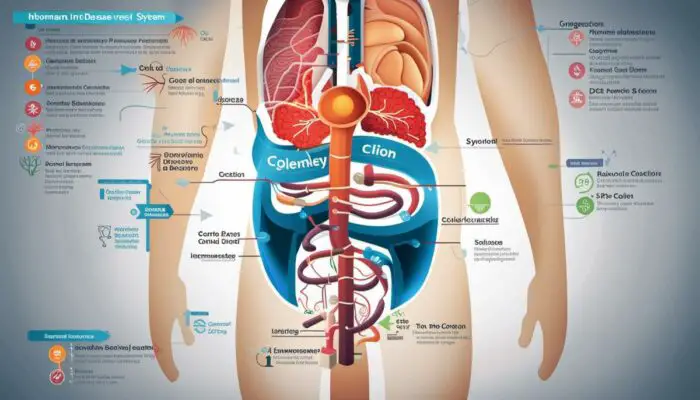
So, Irritable Bowel Syndrome, commonly referred to as IBS, is a chronic condition that impacts the large intestine (colon). The key signs and symptoms often include abdominal pain, bloating, gas, diarrhoea, and constipation. Conversely, some might also experience alternate constipation and diarrhoea.
However, the symptoms usually change over time and may vary in intensity from mild to severe.
Risk Factors of IBS
The exact cause of IBS is unknown, making it a complex condition to fully understand. However, a variety of factors, such as abnormal gut motility, heightened pain sensitivity within the gut, infection, inflammation, and changes in the gut microbiota, possibly play a role in its development.
Furthermore, certain individuals are at a higher risk of developing IBS. Risk factors include being young, female, or having a family history of IBS. Stress and certain types of food can also trigger the symptoms.
*Gluten and Dairy are good examples of this. I do not personally suffer from an intolerance but I have IBS and there have been times that both gluten and dairy have caused flare-ups. I think it has to do with my current health. Days after drinking alcohol I notice these symptoms can be more prevalent but other times I’m fine. I’m sure it is different depending on the individual.
Diagnosis of IBS
The diagnosis of IBS involves an assessment of symptoms and medical history, along with a physical examination. Since there is no specific test to diagnose IBS, the diagnosis is often based on ruling out other conditions that may have similar symptoms, such as Inflammatory Bowel Disease (IBD), celiac disease, and cancer. The Rome IV diagnostic criteria are frequently used in IBS diagnosis, which requires recurrent abdominal pain, on average, at least one day per week in the last three months.
IBS Treatment and Lifestyle Modifications
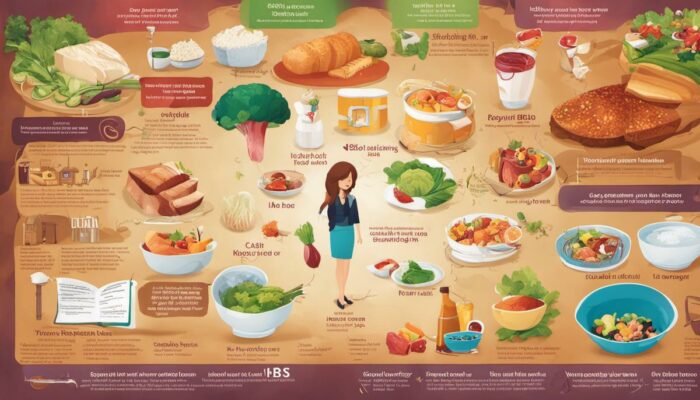
The treatment of IBS usually involves managing the symptoms. Medications may be prescribed to treat severe diarrhoea, constipation, or pain. Dietary changes, such as increasing your fibre intake or avoiding specific foods that trigger symptoms, can also help manage the condition.
Stress management is crucial since stress can exacerbate IBS symptoms. Regular exercise, adequate sleep, and counselling or psychotherapy may also be beneficial.
Distinguishing Between IBS and IBD – What To Look For
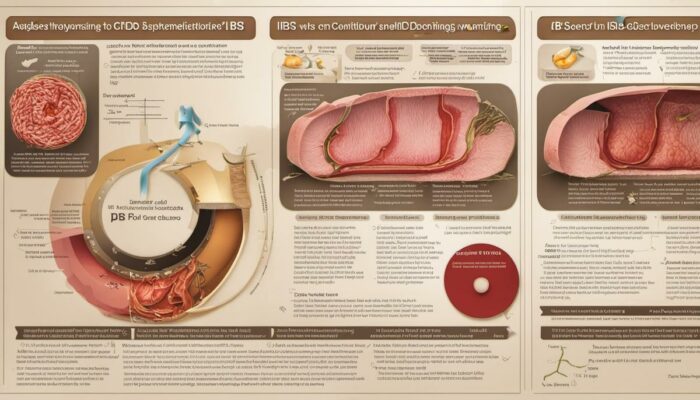
While IBS and IBD can share similar symptoms, they are distinctively different conditions. Unlike IBS, which affects the colon, IBD encompasses various diseases that cause inflammation of the digestive tract, including Crohn’s disease and ulcerative colitis.
Despite the overlap in symptoms such as diarrhoea, abdominal pain, and bloating, IBD also typically involves additional symptoms like blood in the stool, reduced appetite, and weight loss. It’s critical to differentiate these conditions since IBD can result in severe complications.
IBD typically requires more aggressive treatment, such as immunosuppressive drugs and sometimes surgery. Diagnosis of IBD usually involves imaging studies or endoscopic procedures.
Overview
In a nutshell, both Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) are long-standing conditions that affect your digestive system. However, their root causes, how they affect the body, and their treatment methods differ significantly.
Having a comprehensive grasp of these conditions is crucial for accurate diagnosis and effective management.
Understanding IBD
Digging Deeper into Inflammatory Bowel Disease (IBD)
The term Inflammatory Bowel Disease (IBD) is a general label for two primary conditions:
- Crohn’s disease and
- Ulcerative Colitis.
Each of these is characterised by chronic inflammation of the gastrointestinal (GI) tract, leading to ongoing episodes of severe diarrhoea, stomach cramps, weight loss, and fatigue.
The key distinction between the two stems from where the inflammation occurs and its nature. Crohn’s disease has the potential to affect any part of the GI tract from mouth to back passage, while ulcerative colitis confines its effects to the colon and rectum.
Symptoms of IBD
Both Crohn’s disease and ulcerative colitis present varied symptoms that can range from mild to severe. The most common symptoms usually include severe diarrhoea, rectal bleeding, abdominal pain and cramping, reduced appetite and consequent weight loss.
Many individuals may also experience extra-intestinal symptoms such as joint pain, skin issues, eye inflammation, and in severe cases, liver disorders.
Causes of IBD
IBD is thought to result from a combination of genetic, immune system, and environmental factors. In individuals with IBD, the immune system mistakenly attacks harmless bacteria in the gut, causing inflammation and damage. Contrary to popular belief, stress and eating habits, while they may aggravate the condition, are not viewed as primary causes of IBD.
Diagnostic Procedures for IBD
To diagnose IBD, doctors typically rely on various tests including blood tests, stool tests, endoscopic procedures and imaging procedures. Blood tests can highlight possible inflammation and anaemia, whereas stool tests look for signs of infection or blood. Endoscopic and imaging procedures, such as colonoscopy, MRI or CT scans, give a visual confirmation of inflammation and damage.
Treatment Plans for IBD
While there is no cure for IBD, treatments aim to reduce the inflammation that triggers the symptoms, known broadly as ‘inducing remission‘. This is commonly achieved through anti-inflammatory drugs, immune system suppressors, and in some cases, surgery.
As part of this comprehensive treatment, patients may need to alter their diet and lifestyle, to manage symptoms and prevent flare-ups.
IBD vs IBS
The terms IBD and IBS (Irritable Bowel Syndrome) are often confused due to their similar acronyms and overlapping symptoms. However, they are distinct conditions. IBS is a functional disorder, meaning the structure of the bowel is not at fault. Instead, the issue lies in how the digestive system functions. IBS does not cause inflammation, ulcers, or other damage to the bowel, as IBD does.
Additionally, IBS is usually managed with diet and lifestyle adjustments and does not carry the same risk of serious complications as IBD.
Progress in Managing IBD
There have been significant strides in the field of Inflammatory Bowel Disease (IBD) management, thanks to advancements in medical science. For instance, biological therapies have shown promise for individuals who don’t react positively to conventional treatments.
By specifically targeting proteins within the immune system, these treatments effectively decrease inflammation. Additionally, developments in endoscopy, surgical techniques and the implementation of personalised medicine are areas of expertise that appear to offer potential in managing IBD.

Comparing and Contrasting IBS and IBD
A Closer Look at IBS and IBD
Despite the resemblance in their abbreviations, Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) are two different medical conditions. Both of these disorders have an effect on the digestive system, leading to abdominal discomfort and changes in bowel movements.
However, the origin, diagnosis, therapy methods, and complications of these diseases diverge significantly.
Symptoms and Causes
The symptoms of IBS include abdominal pain, bloating, constipation, and diarrhoea. The specific cause of IBS isn’t well-understood. It is considered a functional disorder, meaning the symptoms are real, but there aren’t any visible signs of damage or disease in the digestive tract.
On the other hand, IBD, including Crohn’s disease and ulcerative colitis, is associated with inflammation of the digestive tract, which can result in diarrhoea, bleeding ulcers, abdominal pain, fatigue, and weight loss. IBD is an autoimmune condition where the body’s immune system attacks parts of the digestive tract.
Risk Factors
Risk factors for IBS can include being younger than 45 years old, being female, having a family history of IBS, or having a mental health problem such as chronic stress, anxiety, depression, or a traumatic past such as a history of childhood abuse.
Conversely, risk factors for IBD may include family history, smoking, use of nonsteroidal anti-inflammatory medications (NSAIDS), and living in an industrialised country. Both conditions can adversely affect quality of life and may increase the risk of developing colorectal cancer.
Diagnosis
IBS is typically diagnosed based on symptoms, although doctors can perform tests to rule out other conditions. These can include stool sampling, blood tests, or a colonoscopy. However, there are no specific laboratory or imaging tests that can diagnose IBS.
In contrast, IBD diagnosis includes more extensive tests such as a colonoscopy or sigmoidoscopy, which provide a view of the colon and the end part of the small intestine. They can help determine the level of inflammation, and biopsies can be performed to confirm the diagnosis.
Treatment Options
The treatment for IBS is usually focused on relieving symptoms. This can include changes in diet, medications to control diarrhoea or constipation, and stress management.
IBD treatment typically aims to reduce inflammation which will generally relieve symptoms and prevent complications. Anti-inflammatory drugs, immune system suppressors, antibiotics, pain relievers, iron supplements, and surgery may form part of the treatment plan for IBD.
In Contrast
Despite an apparent similarity in their symptoms, IBS and IBD are distinct in terms of their root causes, diagnostics, and treatment plans. A sound understanding of each and an accurate diagnosis is fundamental for relevant and effective outcomes.
A misdiagnosis or incorrect self-diagnosis can potentially result in improper healthcare, ineffective treatments and an exacerbation of symptoms.
Impact on Quality of Life and Management Strategies
Quality of Life Impact: IBS vs. IBD
Both Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) have significant implications for a person’s everyday life, causing disruption and potentially leading to stress due to the unpredictability of bowel movements affecting social and physical activities.
IBS is a functional disorder impacting mainly the large intestine and manifests in symptoms such as stomach pain, diarrhoea, constipation, and bloating.
Conversely, IBD is an umbrella term including conditions such as Ulcerative colitis and Crohn’s disease, which is a group of conditions causing inflammation throughout the digestive tract.
People diagnosed with IBD might experience weight loss, faecal blood, tiredness, and serious intestine-related complications.
Coping Strategies and Nutrition Tips
Learning to manage IBS and IBD includes both lifestyle alterations and dietary changes. Regular physical exercise and stress-relieving activities such as yoga, meditation or progressive muscle relaxation can help relieve symptoms. Smoking and alcohol are known to exacerbate symptoms and should be avoided.
The role of diet in managing these conditions is elemental. A common approach to controlling IBS is following the low FODMAP diet—avoiding foods rich in certain carbohydrates that are difficult for the gut to digest. IBD often requires a more individualistic diet approach, given its severity and the diversity of symptoms. Nutritionists recommend a diet high in protein and low in dietary fibre to help manage IBD symptoms.
Importance of Mental Health Care
Living with a chronic illness such as IBS or IBD can lead to emotional distress and mental health issues. Depression and anxiety are common among patients dealing with these conditions. Therefore, mental health care plays a critical role in the management of both IBS and IBD.
Cognitive-behavioral therapy (CBT), mindfulness-based therapy (MBT), and other forms of counselling can help manage anxiety and depression associated with these conditions.
Support groups, online or offline, may also be beneficial, as sharing experiences and coping strategies can often help reduce stress and feelings of isolation.
Managing Flare-Ups
Flare-ups, or sudden exacerbations of symptoms, can be particularly distressing. During a flare-up, individuals may find it hard to carry on with their routine due to severe discomfort. A flare-up can usually be traced back to specific triggers such as food items, stress, or lack or too much sleep.
Identifying these triggers and working towards avoiding them can be effective in managing flare-ups. In the case of a flare-up despite preventive measures, patients are advised to rest, stay hydrated and avoid trigger foods while waiting for symptoms to ease.
Lifestyle Management despite IBS and IBD
While living with IBS and IBD can be challenging, these conditions do not have to define one’s life. A well-rounded approach – including dietary management, physical activity, mental health care, and communication with health care professionals – can help individuals navigate their daily lives despite the presence of IBS or IBD. It’s important not to overlook any alarming symptoms and seek prompt medical attention to avoid complications. Regular check-ups and health screenings are also instrumental in managing these conditions.
Regularity, patience, understanding and strength will often prove to be the winning combination in living an enriched life despite IBS or IBD.

Photo by edwardhowellphotography on Unsplash
In Conclusion
The importance of understanding, diagnosing, and managing digestive ailments such as IBS and IBD cannot be understated, as these conditions can drastically shape the contours of an individual’s everyday reality. Bearing in mind the complexities of these disorders, the nuances in their symptoms, and the variance of their effects on different individuals, it is crucial to insist on correct information and communication.
Furthermore, approaching their management holistically, factoring in diet, mental health, and lifestyle alterations can make a substantial difference in coping with these conditions.
This guide serves to equip you with the critical knowledge and practical strategies to navigate these complexities, aiming to empower you to take charge of your health on your terms.
>>>If you would like to read more of our posts about IBS and IBD check out our page HERE<<<


Anxiety and Depression are you magnesium deficient best ways to lower blood sugar BiOptimizers blood pressure supplements blood sugar support supplements Digestive Enzymes Supplement digital products Dr Sam Robbins Exercise Gut Health Healthy Living heart health HFL how to lower blood sugar levels How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance list Magnesium deficiency Matt Gallant mental health multivitamins Nootropics nutrient supplements Oral Healthcare Probiotics Probiotic Supplements proteolytic enzymes reverse type 2 diabetes stress and anxiety stress relief vitabalance vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss tea