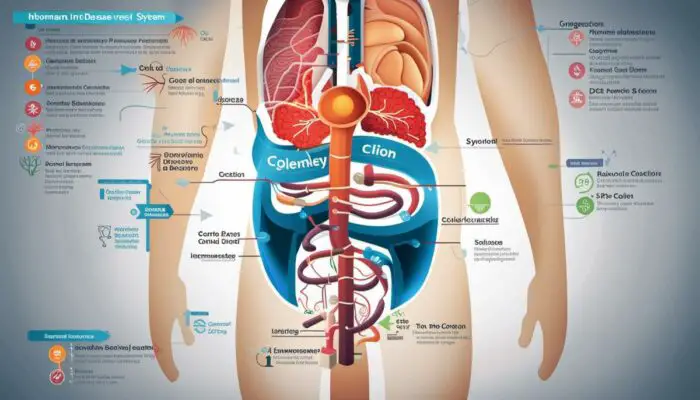
Characterized by a group of inflammatory conditions, Inflammatory Bowel Disease (IBD) inflicts various parts of the digestive tract, with the two most common types being Ulcerative Colitis and Crohn’s Disease. This complexity of disorders bring about a host of complications, from intestinal obstruction to ulcers, that not only affect the physical health of an individual, but impact their mental and emotional wellbeing too.
The importance of understanding, managing, and treating these complications therefore, is critical not just for ensuring physical health, but also for safeguarding mental health.
Delving into the realms of these complications, their management and their psychological implications, this endeavour allots an in-depth exploration into the crevices of IBD fallout.
Understanding Inflammatory Bowel Disease (IBD)
Understanding Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) is a term used to describe two distinct conditions – Crohn’s disease and Ulcerative colitis, both characterised by chronic inflammation of the gastrointestinal (GI) tract. This inflammation can cause severe damage to the GI tract, hindering its capacity to absorb nutrients, effectively digest food and excrete waste.
Types of IBD: Crohn’s Disease and Ulcerative Colitis
Crohn’s disease can occur in any segment of the GI tract, from the mouth to the anus, and can affect the thickness of the intestinal wall, causing deep ulcers and fistulas. On the other hand, Ulcerative colitis is restricted to the colon (large intestine) and rectum, with predominantly superficial inflammation.
Causes of IBD
The exact cause of IBD remains unclear, but it is thought to develop from an inappropriate immune response to environmental factors, in genetically susceptible individuals. For instance, some IBD patients show abnormal immune responses to harmless bacteria present in the intestine. Other factors such as diet and stress may exacerbate these conditions but aren’t necessarily the cause. It’s also worth noting that both forms of IBD can occur at any age, but they’re usually diagnosed before the age of 30.
Symptoms of IBD
IBD symptoms may vary depending on the severity and location of inflammation. Common symptoms include persistent diarrhoea, abdominal pain and cramping, blood in stools, reduced appetite, and unintended weight loss. Apart from GI symptoms, IBD can also have extraintestinal manifestations, including arthritis, skin conditions, and eye inflammation.
IBD Complications
Complications arising from IBD can be myriad and widespread. In Crohn’s disease, for instance, complications may include bowel obstructions, abscesses, fistulas, and anal fissures. In Ulcerative colitis, complications may involve severe bleeding, perforated colon, severe dehydration, and an increased risk of colon cancer.
It’s also essential to understand that IBD can significantly impact individuals’ quality of life, leading to psychological conditions such as anxiety and depression. Therefore, it’s crucial for those living with IBD to seek appropriate medical care and emotional support to effectively manage their condition.
Potential Long-Term Complications of IBD
Those living with Inflammatory Bowel Disease (IBD) may confront several long-term complications. One notable concern could be a heightened chance of developing colon cancer, particularly in those with Ulcerative colitis. In some rare instances, liver damage could also manifest, especially in conjunction with existing liver diseases. Another possible complication is the loss of bone density, otherwise known as osteoporosis, which can be attributed to issues with intestinal malabsorption and the extended use of certain IBD medications.
It should be remembered, however, that each person with IBD has a unique experience with the disease – the progression and complications can vary greatly among individuals. Therefore, a comprehensive understanding of the conditions enables better management and the prevention of potential complications.
Regular communication and planning with healthcare providers plays a fundamental role in dealing with IBD effectively.
Common Complications of IBD
Complication of Intestinal Obstruction
An often-seen complication resulting from Inflammatory Bowel Disease (IBD) is that of intestinal obstruction. This scenario occurs when the intestine becomes blocked, inhibiting the passage of food or liquid. Chronic inflammation can often be the catalyst for this obstruction, leading to scar tissue formation and a subsequent thickening and narrowing of the intestinal wall over time. Typical symptoms may comprise severe abdominal pain, vomiting, bloating, and difficulty in passing gas or stool. In severe instances, an intestinal obstruction can result in the death of a section of the bowel, demanding immediate medical intervention and, most likely, surgery.
Abscesses
Abscesses or infection pockets filled with pus may also develop as a result of IBD. They are often found around the anus or in the lower part of the abdomen. The frequent inflammation and ulceration in IBD can lead to tiny openings in the bowel wall. These openings may allow bacteria to leak out and accumulate, resulting in the formation of an abscess. Abscesses can cause fever, pain, and a palpable mass in the affected area, often requiring drainage or surgery.
Ulcers
IBD can lead to the formation of ulcers, which are open sores in the lining of the digestive tract. These ulcers can occur anywhere from the mouth to anus but are especially common in the large intestine and rectum. The ulcers can cause pain, bleeding, and pus discharge, making digestion and defecation painful processes.
Beyond The Bowel: Other Complications of IBD
Although primarily a condition that affects the intestinal tract, IBD’s impact can extend far beyond the bowel, leading to complications in various parts of the body.
Skin Conditions
IBD patients may develop skin conditions such as erythema nodosum, which presents as tender, red nodules usually on the shins, or pyoderma gangrenosum, a rare condition characterized by large, painful ulcers on the skin.
Eye Disorders
Eye disorders can also occur due to IBD. These may include uveitis, an inflammation of the uvea or the middle layer of the eye, that might cause blurred vision, eye pain and redness; or episcleritis, which affects the outer coating of the white of the eye, causing discomfort and redness, but rarely affects vision.
Joint Pain
Arthritis, or inflammation of the joints, can also occur alongside IBD. It often affects the large joints of the arms and legs, including the elbows, wrists, knees, and ankles, and can cause pain, swelling and reduced mobility.
Liver Conditions
Some people with IBD may experience liver conditions, such as primary sclerosing cholangitis, a condition that causes inflammation, scarring and narrowing of the bile ducts inside and outside the liver. Over time, this can lead to liver damage or cirrhosis.
Bone Loss
Another potential complication is osteoporosis, or bone loss, which can lead to weakened and brittle bones that break more easily. This heightened risk of osteoporosis in IBD patients may be due to the disease process itself, steroid therapy, or nutritional deficiencies.
It is essential to be mindful that the occurrence of potential complications can certainly differ amongst various individuals dealing with this condition. Through regular health check-ups and comprehensive dialogues with healthcare providers, these complications can be promptly identified and adeptly managed.

Photo by erikringsmuth on Unsplash
Management and Treatment of IBD complications
Navigating IBD Complications
Engaging with Inflammatory bowel disease (IBD) and its potential complications often requires an all-encompassing approach, utilising medical, surgical, and lifestyle alterations. The primary aim of treatment is to instigate and sustain remission, principally through decreasing inflammation and adeptly managing the likelihood of complications.
Medical Treatment Options
Medical therapies usually form the frontline approach for managing IBD. These range from aminosalicylates to corticosteroids, immuno-modulators and more recently, biologic therapies. Biologic drugs such as anti-TNF, anti-integrin, and anti-interleukin are used to specifically target and neutralise the inflammatory processes.
Simultaneously, immunosuppressants like azathioprine, mercaptopurine, and methotrexate are utilised to reduce the body’s immune response. However, these have potential side-effects like infection risk and might require regular monitoring.
When it comes to managing acute symptoms such as diarrhoea, pain, and bleeding, aminosalicylates and corticosteroids are used widely. Antibiotics are sometimes used as adjutant therapy, primarily in Crohn’s disease, to manage perianal disease or symptoms from bacterial overgrowth.
Surgical Treatments
Around a third of IBD patients may require surgical interventions at some stage in their life for complications like strictures, fistulas, abscesses or to control refractory bleeding. Resection, strictureplasty, colectomy, proctocolectomy, and ileal pouch-anal anastomosis are some common procedures for IBD. It is worth noting that, whilst surgery can manage complications and often give periods of remission, it is not considered a cure, as disease recurrence elsewhere in the bowel is a common occurrence.
Lifestyle Changes and Proper Nutrition
Self-management through lifestyle modifications can play a crucial role in managing IBD complications. Adopting a balanced diet, rich in proteins, soluble fibre, vitamins, and minerals is recommended while foods triggering flare-ups should be identified and avoided. Regular exercise without overexertion is also beneficial.
Various types of stress can stimulate an IBD flare-up, so stress management techniques, such as mindfulness practice, yoga, meditation or counselling, can be helpful adjuncts to medical treatment. Smoking cessation is highly recommended, as smoking has been linked to worsened disease outcome in Crohn’s disease.
Achieving and maintaining a healthy weight is essential, as both underweight and overweight can worsen the disease course. Thus, a regular dietary review by a registered dietitian is a vital part of IBD management.
The Role of Probiotics and Prebiotics
There is a growing interest regarding the potential role of probiotics and prebiotics in managing IBD, given the role gut microbiota is thought to play in its pathogenesis. However, the evidence is mixed, and therefore, their use should be discussed individually with the treating clinician.
Conclusion
Effectively dealing with treatments for IBD requires a personalized care plan, taking into account the unique conditions of each patient. The importance of ongoing consultation and an open line of communication with healthcare providers cannot be overemphasized in controlling IBD and related complications, ultimately improving the patient’s quality of life.
The Psychological Impact of IBD complications
Mental and Emotional Complications
It’s crucial to note that the complications of Inflammatory Bowel Disease (IBD) go beyond physical ailments, deeply affecting the mental and emotional well-being of those living with it. Suffering from chronic conditions like Crohn’s disease or Ulcerative Colitis can lead to significant psychological complications such as anxiety, depression, and distress. Additionally, the stress from the unpredictability and lifelong nature of IBD can be potentially overwhelming, particularly in the face of public misunderstanding and the associated social stigma around bowel disorders.
Anxiety and Depression
One of the most common psychological impacts of IBD complications is anxiety and depression. The unpredictable nature of the disease, such as constant worry over when the next flare-up may occur, can be a significant source of anxiety. Additionally, IBD patients often feel down due to constant discomfort, changes in their body image after surgery, or the side effects of medication. The fear of having a bowel accident can lead to social anxiety and may result in patients isolating themselves to prevent potential embarrassment.
Effects on Quality of Life
IBD can have drastic effects on a patient’s quality of life. The necessity for continuous medication, frequent doctor’s visits, dietary limitations, and potential surgeries all add to the distress associated with the disease. There can be restrictions on travel due to the need for access to washrooms, which might curb social activities. Not to mention the financial burden that comes with long-term illness. All these factors can make the patient feel trapped, exacerbating feelings of depression and anxiety.
Importance of Mental Health Support
Given how heavily IBD can impact a person’s mental health, support in this area is vital. Psychological counselling, such as cognitive-behavioural therapy (CBT) or mindfulness-based therapy, is proven to be beneficial for those suffering. These therapies can provide patients with coping strategies, improve their disease management, and ultimately their quality of life. Mental health professionals can assist an individual in recognising and altering potentially harmful thought patterns, implementing relaxation techniques, and improving their overall outlook.
The Role of Family and Friends
The support network around a patient, such as family and friends, plays a crucial role in coping with this chronic condition. They are often the bedrock of emotional and psychological support. Encourage open communication about the illness as it not only relieves psychological stress but also enables them to understand the challenges faced and offer the necessary support.
Resources for Mental Health Support
For those who may feel underprepared to deal with the psychological impact of IBD complications, a myriad of resources are available. These may include speaking to “IBD Nurses” who have specialist knowledge in the field and can often provide valuable advice and support.
The Crohn’s & Colitis UK organisation is a resource offering comprehensive information, a confidential helpline, local support groups, and various tools to help manage mental wellbeing. Online forums, such as the IBD Support Foundation, also provide spaces for patients to share their experiences in a safe, supportive environment.

Ultimately, the path of understanding and managing IBD and its complications is paved with complexity and varied challenges. As an individual, ardently familiarising oneself with this malady, its complications, their mitigation strategies, and the psychological impact of enduring IBD can be instrumental in one’s journey towards managing the disease and maintaining a positive outlook.
Deeply intertwined with both physical and emotional spheres of life, proper intervention paired with robust support systems are invaluable. The narrative around IBD needs to be one of courage, strength, knowledge and support, resonating the ethos of a multi-disciplinary approach to embracing and overcoming the trials that IBD imposes. {Read More About IBS and IBD Relief in our articles HERE)