Understanding Pain Management in IBD can be quite challenging, largely owing to the chronic pain that accompanies this health condition. Falling into two main categories – Crohn’s Disease and Ulcerative Colitis, IBD is not just characterized by discomfort but it also significantly distresses patients, as it impairs their overall quality of life. Many with IBD suffer from terrible pain and those that do are desperate for relief.
For this purpose In today’s post, we shall provide a comprehensive insight into the world of IBD, starting with a basic understanding of the disease, the pain associated with it, and its potential causes.
Following a review of current pain management strategies, it explores recent advances in the field, bringing a ray of hope for a potentially better future in IBD pain management.
It also accentuates the profound effect of chronic pain on mental health and offers practical advice to manage the pain and lead a better life despite the fierce nature of IBD symptoms.
Understanding Pain Management For IBD Sufferers
There are many forms of pain management for IBD Sufferers. We shall cover each of these in this article but just to summarize for those that are a bit more eager to know. These include;
- Stress Relief and Management
- Dietary Suggestions and Restrictions
- Natural Remedies and Supplements
- Therapy and Medication
- Exercises and Lifestyle Modifications
Really each can be quite useful to know about. There is certainly much that can be taken away here but just a quick low down on what IBD is and how it affects the human body so…
What Is IBD – A General Overview
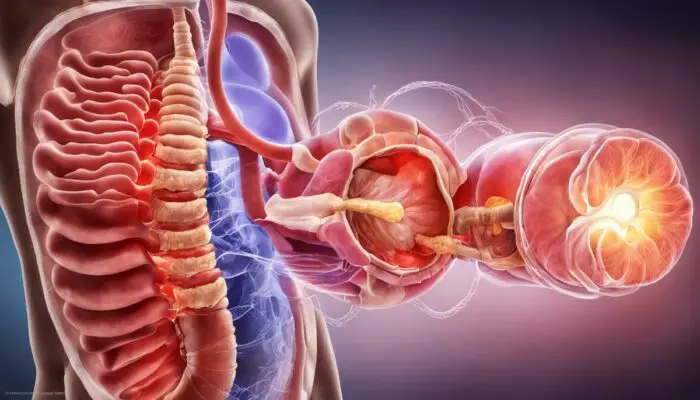
Inflammatory Bowel Disease, commonly referred to as IBD represents a group of intestinal disorders causing prolonged inflammation in the digestive tract.
The common types of IBD encompass Crohn’s Disease and Ulcerative Colitis. The former typically involves inflammation of the lining of any part of the digestive tract, often spreading deep into affected tissues, whereas the latter leads to long-lasting inflammation and sores in the innermost lining of the colon and rectum. Both types exhibit chronic inflammation of the gastrointestinal tract leading to damage that can either be temporary or permanent.
IBD may cause a plethora of symptoms, ranging from mild to severe – largely depending on which part of the digestive tract is affected. Common symptoms may encompass;
- diarrhea,
- abdominal pain and
- cramping,
- rectal bleeding,
- weight loss, and
- fatigue.
The causes of IBD remain unclear; however, it is conjectured that a combination of factors, such as genetics, immune system malfunctions, and environmental elements, could trigger the disease.
The Basic Things To Know About Pain Management in IBD
IBD, or inflammatory bowel disease, is often accompanied by significant pain due to the inflammation and damage it inflicts on the digestive tract. This pain can greatly impact an individual’s standard of living and is often one of the hardest elements to control effectively.
The standard way to manage pain in IBD adopts a diverse strategy, including medication, self-care practices, and medical surgeries where necessary.
In terms of medical treatment, this generally forms the front-line defense in managing discomfort. Doctors often prescribe anti-inflammatory drugs such as aminosalicylates and corticosteroids, with the aim of minimizing inflammation and stimulating remission.
Additional treatments can include immunomodulators and biologic therapies, used to calm the overactive immune response which can help reduce both swelling and pain. Common pain relief drugs like simple paracetamol can also be beneficial, although drugs like nonsteroidal anti-inflammatory ones, known as NSAIDs, are usually avoided as they can actually increase the severity of the condition.
Alongside medication, self-care practices offer meaningful support in managing pain brought on by IBD. Balanced diets, staying sufficiently hydrated, and regular and moderate exercise alongside ensuring sufficient rest can all help to control symptoms. Minimizing stress can also provide its own form of relief.
One reason why many people living with IBD are adopting techniques to manage stress such as mindfulness meditation, yoga, and biofeedback, which can all contribute to the reduction of discomfort and improve the ability to cope with the disease’s associated pain.
For those suffering from severe IBD, surgical intervention can sometimes be required to manage the pain. This could involve the resection, or removal, of the affected part of the bowel in cases of Crohn’s disease, or in cases of ulcerative colitis, sometimes the entire colon may need removing.
While these kinds of surgeries are generally considered the last resort, implemented when other treatments have failed to effectively manage symptoms, they often aim to reduce symptoms, cut down on complications, and improve the patient’s overall quality of life.
As we can see, managing the pain associated with IBD requires a delicate balance of individualized treatments. It is key that anyone living with IBD keeps regular contact with their healthcare provider to help create the most effective pain management plan for their unique condition.
Current Pain Management Strategies in IBD
A Closer Look at Pharmacological Interventions in IBD Pain Management
The pharmacological strategy to manage pain in IBD, or Inflammatory Bowel Disease, typically employs a range of specific medications such as painkillers, anti-inflammatory drugs, and immune-suppressing medications. For starters, your doctor may recommend anti-inflammatory medicines such as aminosalicylates and corticosteroids.
These medications are designed to reduce the discomfort caused by inflammation in the bowel.
If these anti-inflammatory treatments don’t prove successful, your doctor may then prescribe drugs that work to suppress your immune system. These can help in preventing the immune system from initiating inflammation within the gut. Immune suppressor medications include drugs such as azathioprine, mercaptopurine, and methotrexate.
In more severe cases, biologic medicines are used on occasion. These medications function by neutralizing the proteins produced by the immune system. Biologic medications include the likes of infliximab, adalimumab, and certolizumab pegol.
Analgesics, or painkillers, are another common treatment option and can provide effective short-term relief. However, long-term use of these drugs can result in dependence, increased tolerance, and even higher sensitivity to pain, making balance in their use crucial for the patient’s well-being.
Diet Modification in IBD Pain Management
Managing dietary intake is a non-pharmacological yet highly effective approach to managing pain and inflammation in IBD. Due to the varying degrees and types of IBD, it’s vital to note that this isn’t a one-size-fits-all strategy. What works for one person may not work for another.
Notwithstanding, some general diet-related modifications could prove beneficial. These may include avoiding spicy food, limiting the intake of high-fiber foods during a flare-up, and staying hydrated.
It’s also important to limit alcohol and caffeine intake, both of which can exacerbate symptoms.
Foods that are deficient in irritants and high in anti-inflammatory compounds can also be beneficial. These include oily fish like salmon, which is high in omega-3 fatty acids, and fruits and vegetables rich in antioxidants.
Such dietary changes help to maintain gut health and could potentially reduce symptoms and flare-ups.
Utilizing Psychological Therapies to Manage IBD-Related Pain
Inflammatory Bowel Disease (IBD) can have a profound influence on a person’s psychological health. The condition is often linked with heightened stress, anxiety, and depression which, subsequently, can amplify symptom severity and pain perception.
Hence, the implementation of psychological treatments is considered an essential component for managing such pain.
Notably, Cognitive-behavioural therapy (CBT) has been effective in managing pain related to IBD. It aids patients in reassessing and altering detrimental thought processes and behaviors, thereby potentially enhancing pain perception and disease management.
An array of mindfulness-oriented therapies, that concentrate on fostering acceptance and a focus on the present, have demonstrated encouraging results in augmenting suffering-resilience and curtailing pain perception.
This comprises mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT).
Lastly, the significance of support groups and psycho-education must not be overlooked. They offer crucial peer support, alleviate feelings of isolation and misunderstanding, and can contribute to the enhancement of self-care and self-management strategies.

Photo by borndead13 on Unsplash
Recent Advances in IBD Pain Management
Role of Biologics in IBD Pain Management
A crucial breakthrough in pain management for Inflammatory Bowel Disease (IBD) has been the advent of biologic therapy. Biologics, proteins that are derived from human genes and administered via infusion or injection, work towards easing inflammation in the intestinal tract, hence offering relief from pain.
Their method of action involves their capacity to target specific proteins in the body implicated in causing inflammation. Presently, a range of biologics is being employed for IBD treatment, which includes anti-tumor Necrosis Factor (TNF) therapy, integrin receptor antagonists, and inhibitors of interleukin-12 and -23.
These forms of therapy come into play when conventional treatments such as corticosteroids and immune suppressive drugs fail to achieve the desired results.
Gut-Brain Interaction Studies
Gut-Brain Interaction Studies is an emerging field that has been shown to have significant implications for managing pain in IBD patients. This comes from the understanding that the gut and the brain communicate closely with each other, with disruptions in this communication potentially leading to changes in pain sensitivity and perception.
This gives rise to the possibility that treating both the gut inflammation and the psychological factors could be effective in managing IBD pain.
Related Post: IBS and the Gut-Brain Axis Explained
Psychotherapy and Hypnotherapy
Techniques such as Cognitive Behavioural Therapy (CBT) and gut-directed hypnotherapy are increasingly being used to relieve IBD pain. These treatment approaches aim to help patients manage their response to pain, with studies showing that they can lead to significant improvements in pain relief and overall quality of life. CBT, for instance, teaches patients to identify and challenge negative thought patterns and behaviors, which may help to reduce the emotional and physical responses to IBD pain.
Personalized Medicine in IBD Pain Management
The concept of Personalised Medicine or Precision Medicine is gaining ground in the treatment of IBD. This approach involves tailoring treatment to individuals based on their genetic, environmental, and lifestyle factors, rather than a ‘one size fits all’ approach.
The aim is to identify therapies that are more likely to be effective, with fewer side effects, for each individual patient. New technologies, such as genetic sequencing and molecular profiling, are being utilized to better understand the individual patient’s disease and develop a personalized treatment plan.
Medicinal Cannabis and CBD for IBD Pain Management
The use of medical cannabis for pain management in IBD is a fairly recent development. Cannabis contains compounds called cannabinoids which have been shown to reduce inflammation and alleviate pain. Despite the growing acceptance and legalization of medicinal cannabis in some places, further research is needed to establish dosage, safety, and efficacy more precisely.
See Our Recommended CBD Supplements HERE<<
The Path Ahead for IBD Pain Management
The sphere of modern science tirelessly endeavors to bring forth innovative treatments for pain in Inflammatory Bowel Disease (IBD). Recent research has turned its attention to the possible role of dietary adjustments in mitigating inflammation and in turn, easing IBD symptoms.
The advent of virtual reality as a potential therapy represents another step forward, offering respite from pain through distraction. However, any contemplation of these emerging treatments should be accompanied by a thorough dialogue with your healthcare provider for their invaluable assistance and advice.

IBD Pain and Mental Health
The Interplay between IBD Pain Management and Mental Health
Persisting pain, generally of the chronic type, is a regular companion of Inflammatory Bowel Disease (IBD). Grappling with the day-to-day tasks of managing IBD has a significant bearing on an individual’s mental well-being, most notably fostering circumstances conducive to anxiety and depression.
The uncertain trajectory of the illness, coupled with fear of potential flare-ups and the complexity of adapting to a chronic condition, contribute to elevated instances of psychological distress in those living with IBD.
IBD Pain and Quality of Life
IBD pain can significantly affect the quality of life. Chronic, recurrent pain combined with other debilitating symptoms such as fatigue and diarrhoea, can limit daily activities and social interaction.
Thus, people with IBD often feel isolated. Moreover, pain can interfere with one’s career and educational pursuits, providing additional stress.
Depression and Anxiety in IBD Patients
The unpredictable nature of IBD, the frustration of coping with a chronic illness, and concerns about self-image due to physical changes can culminate in psychological issues. A substantial body of evidence supports that IBD significantly enhances the risk for anxiety and depression.
Worrying thoughts around the unpredictability of flare-ups or concerns regarding societal stigma stemming from bowel urgency and incontinence can exacerbate feelings of anxiety. Furthermore, living with chronic discomfort can leave patients feeling downcast and hopeless at times, leading to symptoms of depression.
The Role of Psychological Support
While IBD is a physical condition, the emotional side should not be neglected. Structured psychological support, such as therapy or counseling, can be instrumental in managing the psychological impacts of IBD. It can help individuals better understand and cope with their condition, resulting in improved quality of life.
Specific therapy modalities, like cognitive behavioral therapy, can aid in enhancing coping mechanisms to reduce feelings of stress, depression, and anxiety related to IBD.
Stress Management for IBD Pain
Stress doesn’t cause IBD but can exacerbate symptoms and trigger flare-ups. Stress management therapies, such as meditation, yoga, and biofeedback can prove beneficial for patients in managing not only their stress levels but also their perception of pain.
Some research has indicated the potential benefits of these mind-body therapies in the overall disease course and resolution of symptom flares.
Medication and IBD Pain Management
Disease-specific medication can help control painful IBD flare-ups by reducing inflammation. Depending on the severity of the condition, pharmacological therapy can vary from aminosalicylates, and corticosteroids, to biologic therapies.
Surgical Interventions
In severe cases, surgery may be a solution to manage chronic pain in certain types of IBD. Surgery can remove the diseased part of the bowel, reducing or eliminating the pain.
Pain Management in IBD and Its Effect on Psychological Wellbeing
It is fundamental to recognize chronic pain and its ensuing psychological issues as crucial components of IBD management. Utilizing a multidisciplinary strategy that includes primary care doctors, gastroenterologists, pain specialists, and psychologists, may prove to be the most favorable approach to managing and enhancing the overall quality of life for those afflicted with IBD.

Practical Tips for IBD Pain Management
Inflammatory bowel diseases (IBD), broadly classified as Crohn’s disease and ulcerative colitis, are enduring conditions impacting the digestive system. One of the most common indicators of IBD is recurrent abdominal pain, which can be alleviated through various pain management strategies.
This involves a comprehensive approach that merges medical treatments and lifestyle alterations.
Emphasizing a healthier lifestyle can play a crucial part in controlling IBD pain. Regular physical activity may aid in reducing stress levels, promoting mental health, and enhancing the overall functionality of the digestive system. However, strenuous workouts should be avoided during flare-ups to prevent exacerbating pain and other symptoms.
Getting ample sleep is also essential. Sleep deprivation can amplify pain perception and induce IBD flare-ups. Hence, establishing a regular sleep schedule and practicing good sleep hygiene can significantly contribute to IBD pain management.
The role of diet in IBD is complex and individual-specific, given how different foods can trigger inflammation and symptoms in different people. Whilst there are no uniform diet recommendations for IBD, general advice includes staying hydrated and maintaining a balanced diet.
Some individuals may benefit from a low-residue or low-fiber diet during flare-ups to limit bowel movements and thus, reduce pain. It may be beneficial to consult a dietitian for personalized advice.
Keeping a food diary can help identify potential trigger foods to be avoided.
Stress and anxiety can aggravate IBD symptoms, including pain. Therefore, integrating relaxation techniques such as yoga, deep-breathing exercises, and mindfulness meditation may be beneficial. These practices encourage stress reduction and promote a sense of well-being which, in turn, can help manage IBD symptoms.
Psychotherapy or cognitive behavioral therapy can also be considered. These forms of therapy are effective for managing stress and improving coping mechanisms for chronic conditions like IBD.
Living with IBD can take a psychological toll, which can exacerbate physical symptoms. Connecting with support networks—whether online communities, support groups, or counselors—can be immensely helpful. Sharing experiences, gaining insights, and realizing that one is not alone in their struggle can bring solace and encouragement.
Combining medical intervention, lifestyle adjustments, and supportive therapies can empower people with IBD to take control of their pain management. It’s always important to have open communication with healthcare providers to ensure any changes align with medical advice.

In Conclusion
Pain management in IBD is complex but not impossible. Emerging strategies promise a more personalized and effective approach, demonstrating the value of biologics, an understanding of gut-brain interactions, and more. Whilst medical interventions are crucial, there’s no underestimating the importance of simple yet significant lifestyle modifications in managing IBD pain.
Diet changes, stress reduction techniques, and seeking psychological support can truly make a difference in improving the quality of life. The fight against IBD pain is not just about science and medications, but also about resilience, adaptability, and emotional well-being.
As we continue to learn more about this condition and its management, individuals with IBD and their loved ones can look forward to a future where they gradually reclaim their lives from the clutches of pain.
>>>Read More of Our Articles About IBS and IBD Relief HERE<<



Anxiety and Depression best ways to lower blood sugar BiOptimizers blood pressure supplements blood sugar support supplements Digestive Enzymes Supplement digital products Dr Sam Robbins Exercise Gut Health Healthy Living heart health HFL how to lower blood sugar levels How To Lower Cholesterol insulin resistance joint health supplement Keto keto dieting Keto Diet Weight Loss leaky gut supplements leptin resistance list Magnesium deficiency Matt Gallant mental health multivitamins Nootropics nutrient supplements Probiotics Probiotic Supplements proteolytic enzymes reverse type 2 diabetes stress and anxiety stress relief vitabalance vitamin c vitapost Wade Lightheart weight loss articles weight loss diet plans weight loss product reviews weight loss supplements weight loss supplements that work weight loss tea