Inflammatory Bowel Disease (IBD) – a term many may be unfamiliar with, yet for those who have been diagnosed, it’s a reality they live with day in and day out. Underpinning the more widely known maladies of Crohn’s Disease and ulcerative colitis, IBD is a chronic condition that carries with it profound life altering implications.
Within this discourse, we will build a comprehensive understanding of IBD, its causative factors, and symptoms – cementing our comprehension of why medication is a requisite component of management. We will then traverse the landscape of available IBD treatments – dissecting aminosalicylates, corticosteroids, immunomodulators, and biological therapies.
Additionally, we cast a spotlight on the deciding factors that assist in shaping personalised treatment plans. Ultimately, we aim to provide practical insights and advice to those living with IBD and managing their medication.
Understanding IBD Medications: A Comprehensive Guide
Understanding Inflammatory Bowel Disease (IBD)
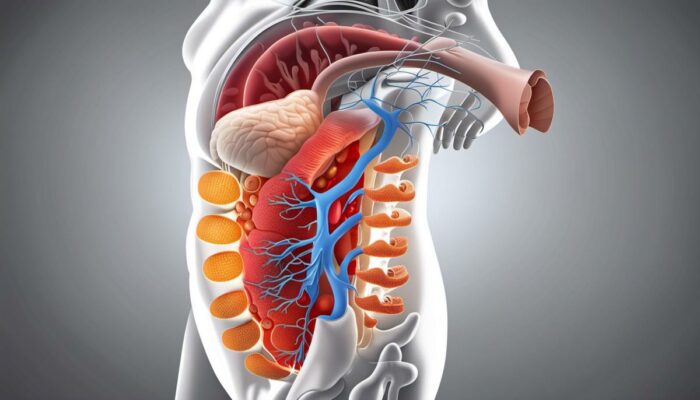
Inflammatory Bowel Disease (IBD) is a broad term that describes chronic inflammation of the digestive tract. Two primary types of IBD exist: Crohn’s disease and Ulcerative colitis. Although sharing many similarities, these two conditions affect different regions of the gastrointestinal tract.
Crohn’s disease is characterised by patchy inflammation that can affect any part of the digestive tract, from the mouth to the anus. Notably, it often impacts the lower part of the small intestine, known as the ileum. On the other hand, Ulcerative colitis primarily causes inflammation and ulcers in the colon and rectum, which persistently bleed and produce pus.
Common symptoms of IBD include persistent diarrhoea, abdominal pain, rectal bleeding, weight loss, and fatigue. Some individuals may also experience less common symptoms such as joint pain, skin conditions, eye inflammation, and liver disorders.
The exact cause of IBD remains unknown. However, research suggests that several factors might contribute to development of the condition. These include genetics, a malfunctioning immune system, and environmental factors. IBD tends to affect those aged 15-35 years old, though it can develop at any age, and it appears to be more common in developed nations and urban areas.
The Role of Medication in IBD Management
The ongoing nature of Inflammatory Bowel Disease (IBD) often necessitates prolonged medication to manage its symptoms, avert complications, and uphold a satisfactory quality of life. A suitable treatment regime generally includes reducing inflammation, managing symptoms, and warding off disease flare-ups. Bear in mind that the treatment methods are tailored to each individual, reflecting the severity of the disease and the patient’s overall health.
The initial medicinal approach to IBD usually includes anti-inflammatory drugs such as 5-aminosalicylates and corticosteroids, working to reduce inflammation in the gut. For more resistant or severe cases, immunosuppressive drugs like azathioprine or biological agents like infliximab may be employed. These medicines alleviate symptoms by subduing the excessive immune response that characterises IBD.
Occasionally, antibiotics are administered to tackle bacterial overgrowth in the small intestine caused by inflammation. Similarly, nutritional supplements and vitamins may be required to tackle deficiencies resulting from malabsorption, a common complaint in IBD patients. In some particularly severe cases, surgical intervention may become essential.
Adherence to the prescribed medication is crucial in effectively managing IBD and minimising the risk of severe complications such as bowel obstruction, abscesses or fistulas, and an elevated risk of colon cancer. It’s also crucial to remember that although medicine can manage symptoms and prolong remission, there is currently no definitive cure for IBD.
Scheduled check-ups are an integral part of IBD management, allowing doctors to track disease progression, assess therapy effectiveness, detect any adverse effects, and make necessary treatment adjustments.
Successful IBD management necessitates a full-scale approach, incorporating medication, diet changes, psychological well-being, and supportive care. The definitive objective should be to instigate and maintain prolonged remission, thus enabling individuals with IBD to lead rewarding, active lives.

Types of IBD Medications
Understanding Aminosalicylates
Aminosalicylates, known colloquially as 5-ASAs, encompasses medications such as sulphasalazine, mesalamine, balsalazide, and olsalazine. These drugs serve as a primary treatment for mild-to-moderate ulcerative colitis, their objective being to mitigate intestinal inflammation by blocking the substances causing it. Depending on which part of the intestine is affected, they can be administered orally, topically or rectally. Side effects could include nausea, diarrhoea, abdominal cramps, and headaches.
Corticosteroids
Corticosteroids, such as prednisolone, hydrocortisone, and budesonide, are potent anti-inflammatory drugs used for moderate to severe flare-ups of IBD. Typically, they’re employed only for short-term use, as long-term use can lead to severe side effects including weight gain, osteoporosis, glaucoma, and increased vulnerability to infections.
Immunomodulators
Immunomodulators, including azathioprine, mercaptopurine, and methotrexate, work by dampening the activity of the immune system, thereby reducing the inflammation in the digestive tract. These drugs are typically used where aminosalicylates and corticosteroids have failed, or to maintain remission in patients who rely on corticosteroids. Some of the potential side effects include liver damage, nausea, and an increased risk of infection.
Biological Therapies
Biological therapies, or biologics, are a newer class of IBD medications that work to suppress the immune system. These include drugs like infliximab, adalimumab, and vedolizumab. They target specific parts of the immune system to reduce inflammation and are typically administered through injections or infusions. Side effects may include infections, allergic reactions, fatigue, and potentially an increased risk of certain cancers.
Surgical Treatments
When medication isn’t effective or side effects become unmanageable, surgery may be considered. This can involve the removal of damaged parts of the intestine or the creation of a stoma (an opening on the abdomen where waste can be expelled). These surgeries can often improve symptoms significantly, but also carry risks of complications and require lifestyle adjustments.
In conclusion, there is a variety of medication available for Inflammatory Bowel Disease (IBD) treatment, each with its unique advantages and inherent risks. Consequently, the choice of therapeutic intervention is personalised, taking into consideration multiple factors such as the severity and distribution of the disease, complications, existing comorbidities and personal patient preferences. It is of utmost importance to consult a healthcare professional to enable a thoroughly informed decision.

Factors Affecting Choice of Medication
Determining Disease Severity
The intensity of Inflammatory Bowel Disease (IBD) is a crucial factor in deciding the most appropriate medication for a patient. For those with a mild form of the disease, a class of anti-inflammatory drugs known as aminosalicylates may provide adequate relief. Conversely, individuals grappling with a severe manifestation of IBD may require more potent medications such as corticosteroids, immunomodulators, or even biological drugs which specifically target certain proteins linked to inflammation.
Patient’s Age and Overall Health
The age and overall health status of the patient is another component that plays a significant role in deciding the appropriate medication. For example, certain types of strong medication, such as corticosteroids, are not suitable for older patients due to the increased risk of side effects, including osteoporosis. Such medications may also not be ideal for patients with poor overall health. On the other hand, healthier and younger patients might benefit from them.
Patient Lifestyle
The lifestyle of the patient is also considered when selecting medication. If a patient leads an active lifestyle and doesn’t want to deal with the inconvenience of needing to take medication multiple times a day, the doctor may prescribe drugs that are only required to be taken once daily. The patient’s job can also factor into this decision, for instance, if they travel frequently or maintain irregular eating patterns.
Cost of Medication
The financial implications cannot be ignored when determining the best treatment plan for IBD. Medications like biological therapies can be expensive, making them unviable for patients who cannot afford them without substantial financial assistance or coverage. The healthcare provider’s decision might also be influenced by the price of these drugs, considering the high healthcare costs and the potential financial burden on patients.
Treatment Personalisation
Deciding on the correct treatment plan for IBD is not a straight-forward process. It is a personalised approach that takes into account the individual’s circumstances, needs, and preferences. Each patient’s condition, financial situation, attitudes towards their health, and personal lifestyle are considered in-depth before a doctor formulates the best possible treatment plan.
Linked Co-Conditions
Patients with IBD often have linked co-conditions such as arthritis, skin and eye conditions, or liver disease, that also need to be treated. The medication chosen should not interfere with the treatment of these conditions, and where possible, may also help treat the additional symptoms. For example, if a patient with IBD also has arthritis, a biological medication like Adalimumab would be recommended as it treats both conditions.
Assessing Side-Effects and Risks
When musing over a medication choice, a salient part of that decision revolves around the possible side-effects and dangers linked to certain drugs. It is not uncommon for some patients to veer towards a safer albeit less potent medication, as they are reluctant to take risks.
Added to that, the fallout from medication side-effects potentially infringes upon the quality of life. For instance, medications such as Prednisolone, if administered for extensive periods, could instigate substantial mood variations and weight gain.
Consequently, a comprehensive discussion encompassing potential side-effects and associated risks with the patient is an essential precursor to reaching a finalised treatment strategy.
Living with IBD: Managing Your Medication
The Imperative of Sticking to Prescribed Medication
A key facet of managing Inflammatory Bowel Disease (IBD) lies in grasping the regimented nature of the prescribed medication and sticking to it diligently. This bespoke prescription is an outcome of careful consideration from the physician, factoring in the patient’s medical history, severity of disease, and associated risk elements. A departure from the plan could potentially spark a resurgence of symptoms or exacerbate the risk of complications.
Importantly, even if there is a marked improvement in symptoms, it is vital to carry on with the medication as prescribed. Stopping treatment prematurely could not only pave the way for a relapse but also intensify the severity of the disease. It’s a common temptation among patients to reduce their dosage or break off their medication regimen once they start to feel better, but it is crucial to maintain an open line of communication with healthcare providers before deciding to modify the medication plan.
Dealing with Side Effects
Medications for IBD can sometimes cause uncomfortable or tricky side effects, ranging from nausea to fatigue or insomnia. However, it’s significant to bear in mind that these side effects are usually temporary and will recede over time. It is also worth noting that the balance between the benefits and risk of these drugs leans overwhelmingly in favour of their benefit, particularly for those with moderate to severe disease.
If side effects persist or become intolerable, patients should engage with their healthcare providers to discuss possible alternatives or modifications to the medication regimen. Often a simple adjustment can alleviate discomfort without compromising the effectiveness of the therapy.
Organising Medication
With a condition like IBD, medication can become a significant part of everyday life. Therefore, being organised can prove beneficial in preventing missed doses. Practical tips include setting reminders on phones, using a pill organiser, and maintaining a medication journal. Storing the medication in a frequently visited area might also serve as an effective visual reminder to take the medicine.
Interacting with Health Care providers
Communication with healthcare providers is vital in managing IBD medications. Remember to share any adverse experiences related to the medication, no matter how insignificant they might seem. It allows the provider to adjust the treatment plan accordingly and provide the best care possible.
Healthcare providers should be a wealth of information, offering guidance on administering the medication, managing potential side effects, and answering any related questions or concerns. Utilise these resources as much as possible to ensure you’re receiving the optimum care and management for your IBD.
IBD Medication: Real-life Experiences and Advice
Lifestyle changes, diligent adherence to medication, and regular communication with healthcare providers are all possible ways that individuals have found they can live comfortably even with IBD. Additionally, many have found benefit from support groups, where they can connect with others going through similar experiences. These lived experiences resonate closely with the expert advice provided by medical professionals and reaffirm its validity.
Sharing these experiences and advice within the IBD community can help others to feel less alone, providing comfort and motivation to continue with their medication regimen. Fostering a sense of communal support could, in the long run, enhance the overall management and understanding of the disease.

Without a doubt, navigating the world of IBD can be an odyssey, but with adequate knowledge and the right tools, one can feel equipped to face the challenges head-on. Every individual’s journey with IBD is distinctive, coloured by different symptoms, responses to treatments, and life circumstances.
However, one universal shared experience is the necessity for medication and often its accompanying side effects. Understanding the different types of medications, their operation, and potential side effects can empower individuals, allowing them to make informed decisions in concert with their healthcare providers.
In the process, the importance of adherence becomes evident, as does the significance of having an organised approach to medication management. Ultimately, facing IBD is not a journey anyone should embark on alone, and through this discourse, we hope to feel more akin companions in your journey.